Automate insurance claim process save 40% of your admin’s time.






The Healthcare Revenue Cycle Management/TPA management process serves as a vital bridge between insurance companies and hospitals. Within this intricate system, Ezovion offers invaluable support by streamlining internal operations. From payer and patient management to processing both planned and emergency claims with proper step-by-step processes by ensuring seamless workflow. Our services encompass meticulous documentation for future reference, ensuring comprehensive and efficient healthcare management.
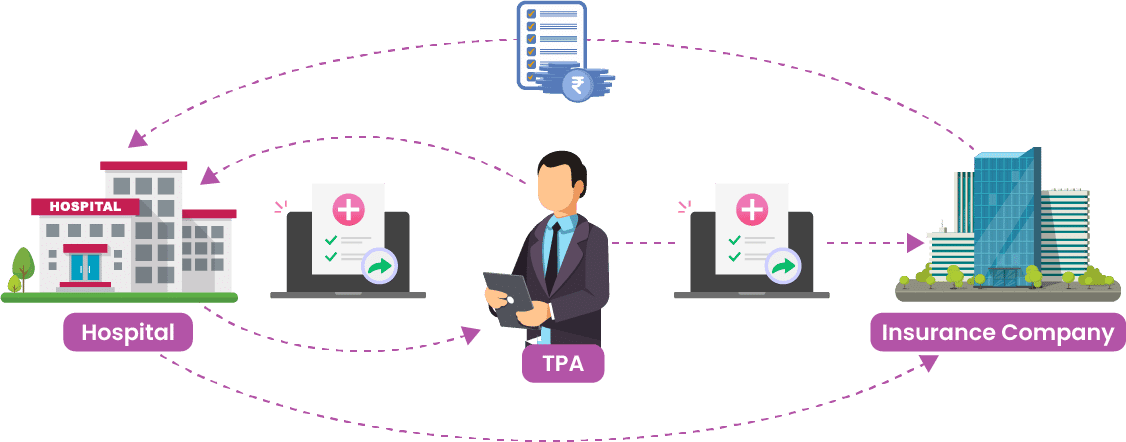
Enhance efficiency by integrating Healthcare Revenue Management Cycle/TPA in medical insurance to ensure a smooth approach to insurance claim process management solutions. Speed-up your insurance claims processing, payer, policy administration, claim document and data management which can improve overall process efficiency.
The Healthcare Revenue Cycle Management Healthcare / TPA in medical insurance helps hospitals manage payers, ensuring effective collaboration and communication. Accurate and secure handling of patient information, enhancing the enrolment process and maintaining comprehensive profiles for error-free claim processing.
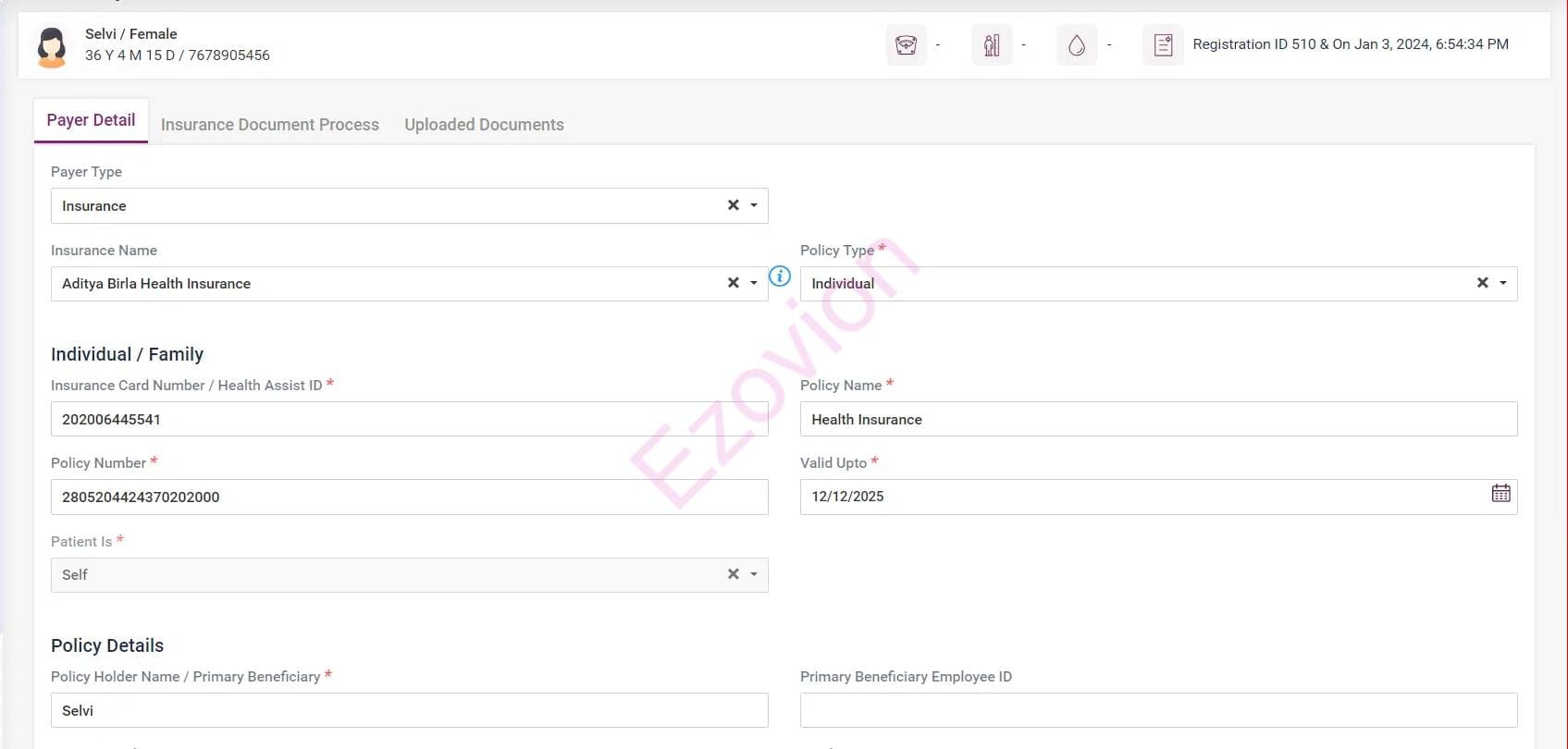
Manage payer details, and activate or deactivate payers.
Payer-wise rate management for easy and accurate billing processing.
Track your patients with a payer with just one click.
Our Healthcare Revenue Cycle Management software supports planned or emergency admission claim processing or you can customize your claim process according to your requirements.
Helps to complete pre-authorization, admission, treatment, and discharge for planned admissions.
Get admitted, pre-authorization by the hospital, treatment, and discharge in case of emergency admissions.
Generate reports based on admission/claim type for efficient claims tracking, claim management and faster settlement.
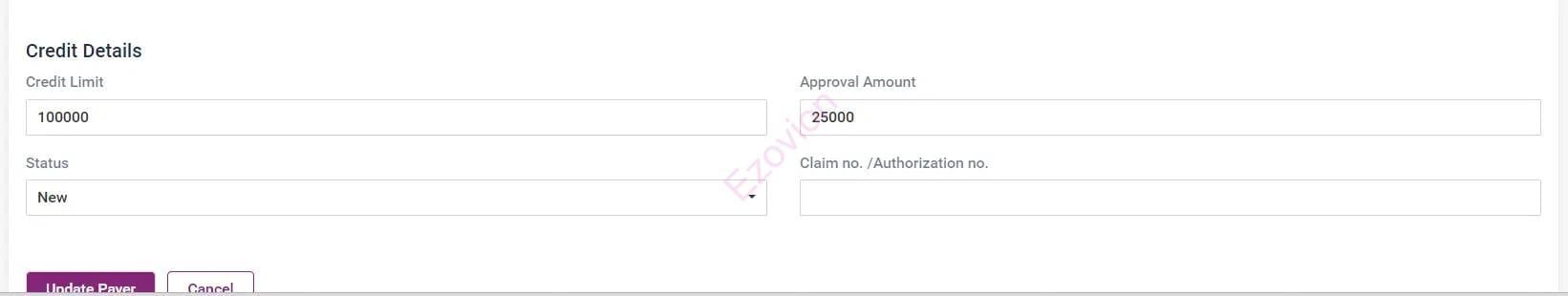
After the patient is admitted, document their eligibility, enrollment status, policy coverage, deductibles, approved services, and limits for quick and efficient tracking and settlement.
After the claim is authorised, the claim number will be assigned.
Update pre-authorised data, upload all pre-authorised process documents.
Notify the patient if the patient is not eligible for benefits.
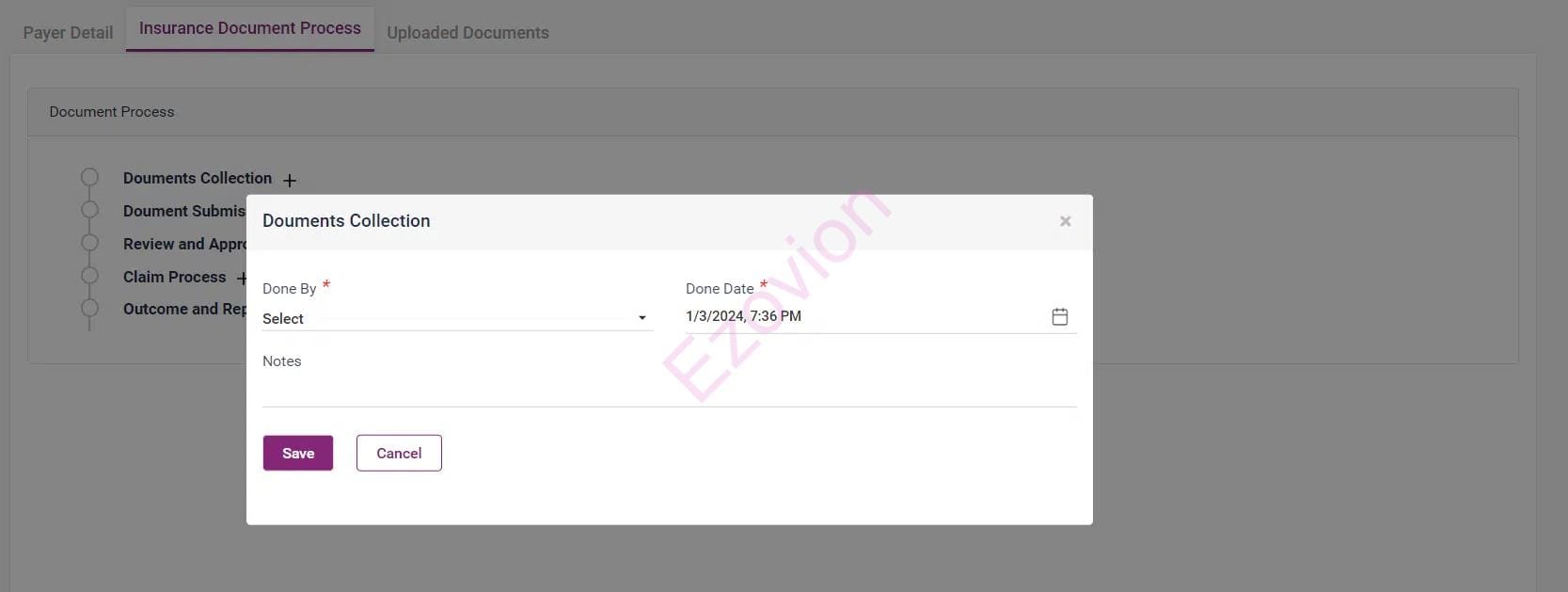
After the admission of the patient, initiate uploading documents for storing, and retrieving essential documents related to every Healthcare Revenue Cycle Management/TPA interaction and claim processing.
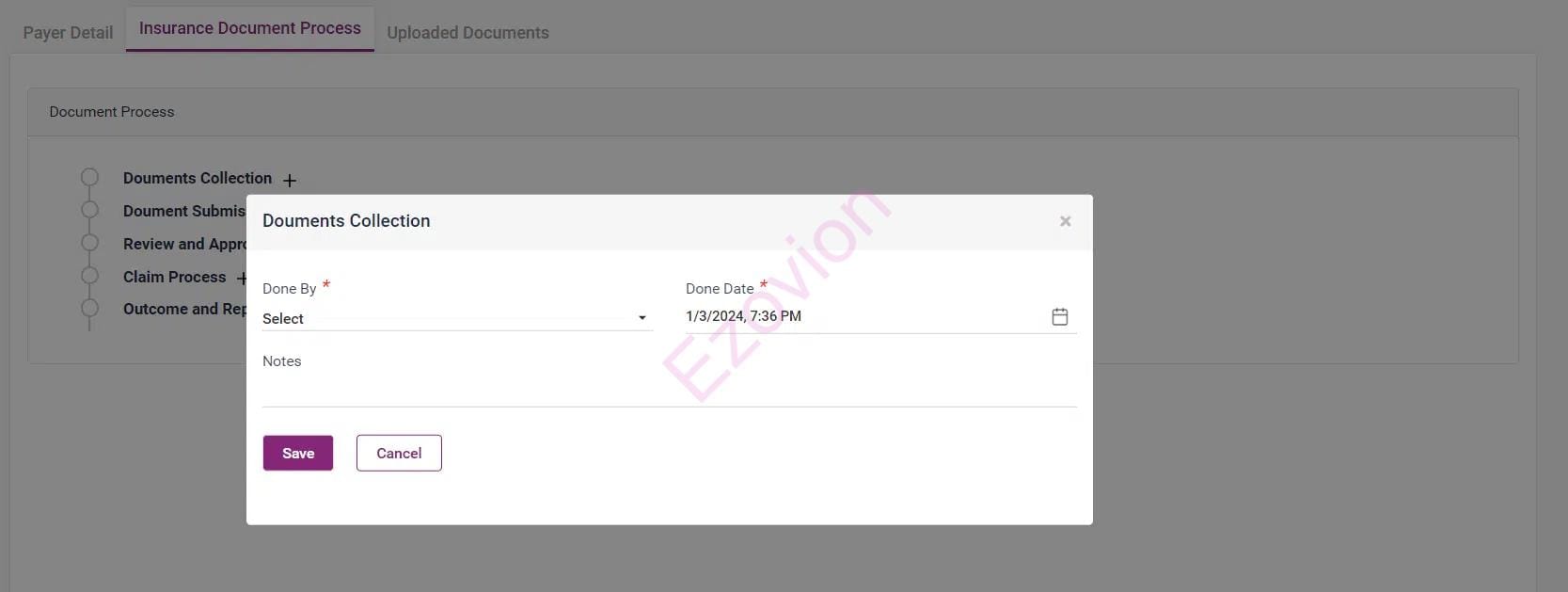
Manage and store claim process required documents.
Documents are stored in a secure system to retrieve when needed and for an efficient audit trail.
Maintain compliance and identify any irregularities in the claims process.
After a patient is discharged, our revenue cycle management in medical billing assists you in recording each phase, from claim submission to bill adjustments and claim adjudication.
Upload essential documents like discharge summaries, investigation reports, pharmacy bills, OT implant invoices, and hospital invoices.
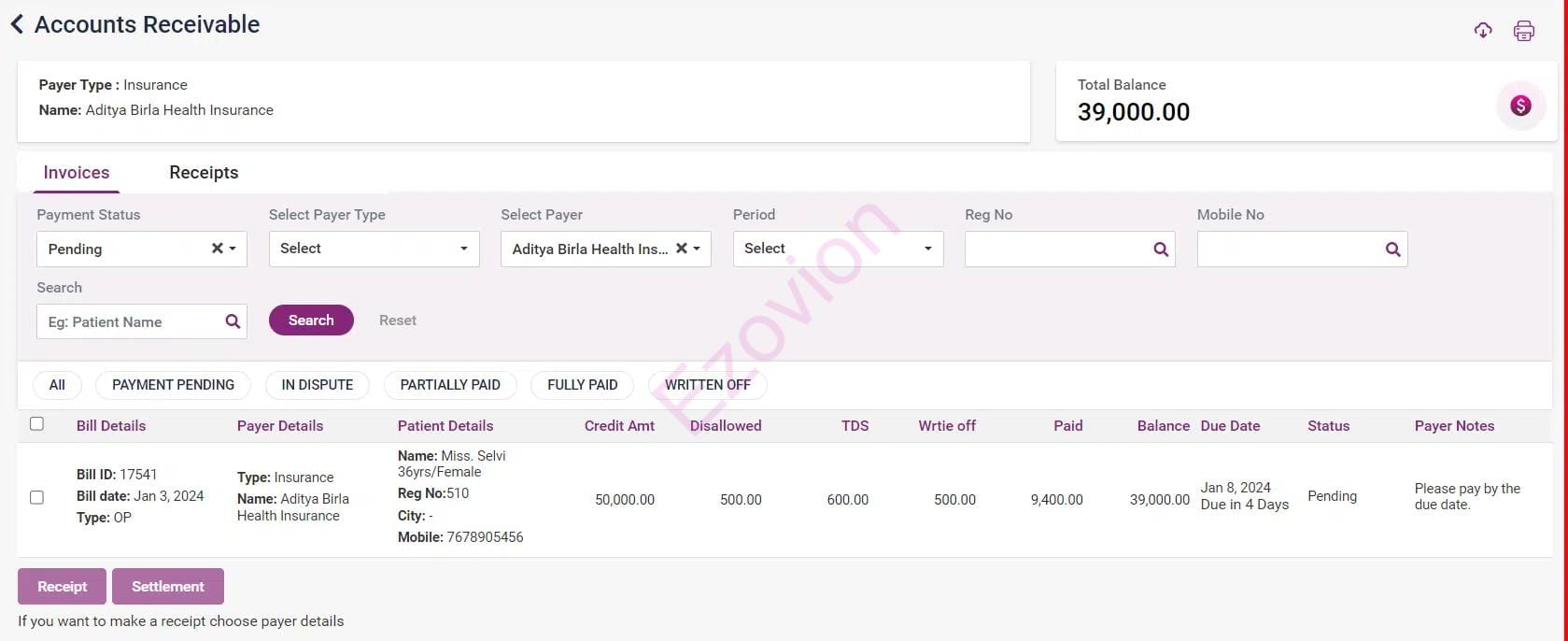
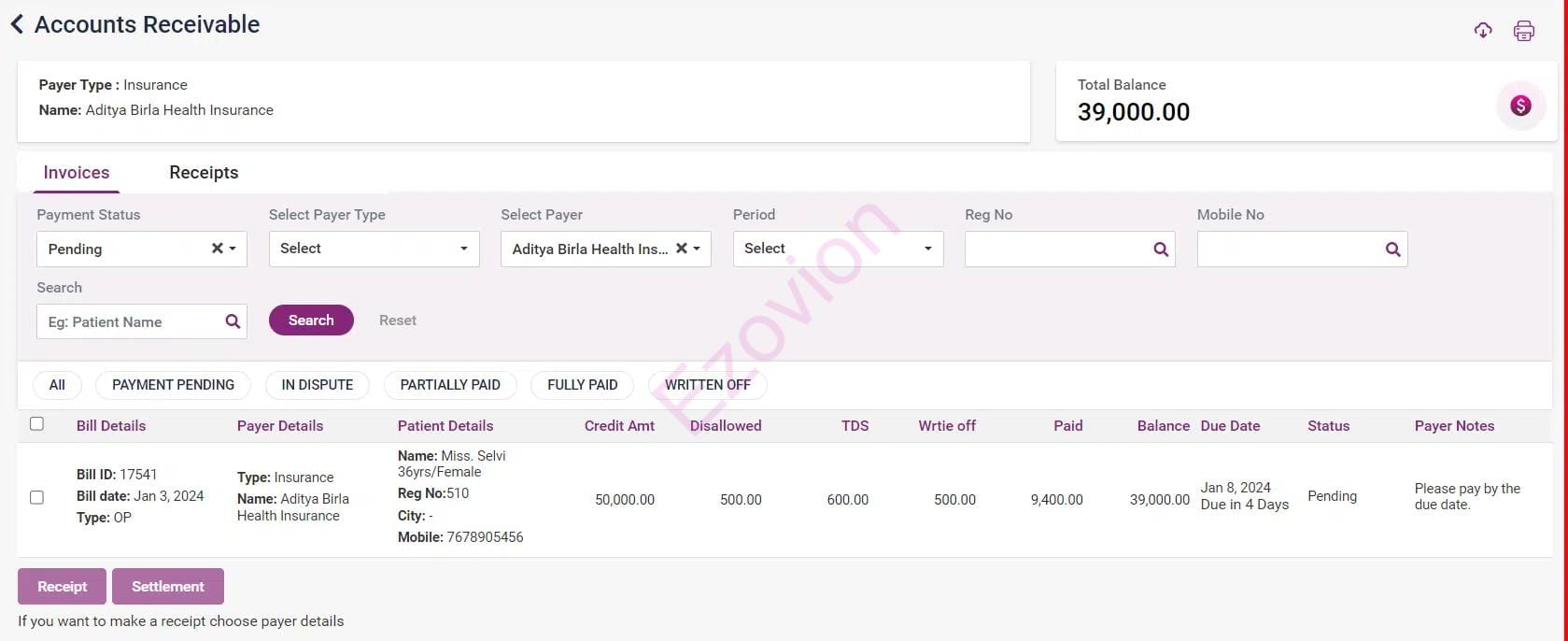
Modify payment terms as necessary, and manage settlements, disputes, and generate reports. See screenshots for a visual overview.
Provision to correct missing or incomplete information for the claims requires additional scrutiny; Appeal denied claims.
A comprehensive audit trail is maintained to track changes and decisions made during the adjudication process.
Revenue cycle management in medical billing allows the claim adjudication process, reducing errors and expediting the assessment of claims for quicker resolutions.
Record the payment method and details from the payer’s claim payment, along with any remaining outstanding balance. Additionally, document appeals on claims, if necessary, by supplying additional information and arrive at a final determination.

Claims status is updated automatically, accounts receivable, and payment management.
The software allows you to mark disallowed invoice items, write-offs, or waiver of pending dues, claim statuscloses and reporting.
The system aids in account reconciliation by tracking billing, payments, and other financial transactions, promoting accuracy and transparency.
Healthcare Revenue Cycle Management/TPA processes starting from claim initiation to get the payment closed, needed lots of communication between all the stakeholders for faster accounts receivables.
TPA software Integrated with the HIMS system gives you a holistic way of communication.
Comprehensive claim data management helps efficient communication.
SMS integration for real-time communication.
Ezovion HIMS offers robust reporting and dashboard features, providing hospitals with insights into their Healthcare Revenue Cycle Management/TPA interactions, claims status, and financial metrics.
Our HIMS incorporates a tracking tool to monitor the status of claims, ensuring that each stage of the process is efficiently managed and reported.
Payer-wise inpatient list and claim reporting.
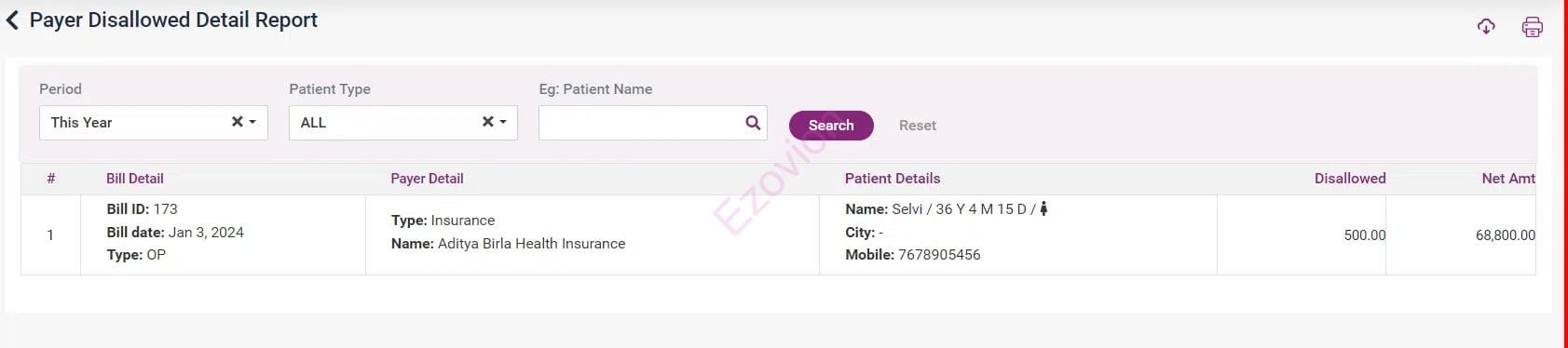
Payer Disallowed Detail Report, TDS Ledger, Dispute bill list.
Write-off list, Live claim status reporting, Track and isolate frequent disallowed items, Aging reports.

The entire Healthcare Revenue Management Cycle/TPA management process acts as a link connecting insurance companies and hospitals. In this process, Ezovion can assist you in organizing internal tasks such as managing payers and patients, handling planned and emergency claims, and overseeing documentation for future reference.
A powerful Third-Party Administrator (TPA) or Healthcare Revenue Cycle Management service that allows healthcare providers to focus on delivering quality care while ensuring a smoother and more reliable reimbursement process.
It is essential to recognize that third-party administrators/Healthcare Revenue Cycle Management function as intermediaries between the insurance company and the policyholder. Consequently, they may not possess exhaustive information, as they are not the ultimate decision-makers. While they assist in claims settlement and investigations, the final approval or denial of a claim rests with the insurance company.
No, Healthcare Revenue Cycle Management/TPAs and agents serve distinct roles. Insurance agents comprehend your coverage needs and assist in selecting the most suitable policy. On the other hand, TPA in medical insurance functions as intermediaries handling various policyholder-related responsibilities.
The services offered by Healthcare Revenue Cycle Management/TPAs are integral components of your insurance plan. There is no requirement to make additional payments for TPA in medical insurance services.