



Complex documentation in healthcare can lead to inefficiencies, errors, and delays that hinder patient care. That’s where our standardized HMS templates come in! Check out our 3 versions of purpose-built templates that easily capture comprehensive information while keeping it concise. This allows providers to spend less time on documentation and more time on what really matters—caring for their patients.
An OP Bill is an essential document that details the healthcare services provided to an outpatient, outlining costs for consultations, diagnostic tests, and medications. It ensures transparency in healthcare transactions, assists with insurance claims, and serves as a future reference.
Key Components of an OP Bill:
The patient’s information is fundamental to the OP Bill. It includes the full name, age, gender, contact details, and address. This information is vital for linking the bill to the patient’s medical history and ensuring accurate billing, thus minimizing potential errors.
Example: The bill identifies the patient as “Mr. Anil Kumar, 45 years old, residing in Whitefield, Bangalore.”
The OP Bill must clearly specify the healthcare facility or provider. This includes the name, physical address, contact numbers, and relevant identifiers such as GST numbers. Providing this information establishes accountability and helps the patient know where to direct any billing inquiries.
Example: The bill is issued by “ABC Medical Center, located at 123 MG Road, Bangalore,” serving as a reliable reference point for the patient.
The bill should document details regarding the consultation, including the physician’s name, specialty, and any relevant treatment information. This ties the services rendered to the patient’s care, providing a transparent view of the healthcare professional responsible for their treatment.
Example:The attending physician for this case is “Dr. Meera, a specialist in internal medicine,” linking the consultation directly to her expertise.
Every OP Bill must display a unique bill number along with the date of issuance. These elements are critical for tracking the transaction, whether for insurance claims, follow ups, or hospital accounting. A reference number aids in easy retrieval for any future queries.
Example: The bill was issued on “24/09/2024” with a unique reference number “#67890,” ensuring straightforward financial tracking.
A transparent OP Bill will include an itemized list of all services rendered and medications prescribed, detailing quantities and individual pricing. Each item must be clearly described, eliminating ambiguity regarding charges. This detail allows patients to understand the nature of the services provided and manage their healthcare expenses effectively.
Example: The bill lists services such as “General Consultation and Blood Test,” each with its associated costs.
The OP Bill should clearly outline any applicable taxes, including Goods and Services Tax (GST). By detailing the Central GST (CGST) and State GST (SGST), the bill ensures patients are informed about government charges. Discounts, whether for specific services or promotions, should be transparently included to reflect the net payable amount.
Example:In this case, a 6% CGST and 6% SGST were applied, ensuring clarity in tax calculations.
It is essential for the OP Bill to clearly state the total amount due. Patients should easily identify the gross amount, any deductions, and the final payable sum. Additionally, indicating the payment status (paid or due) and the payment method used (cash, credit card, insurance, etc.) simplifies the transaction and prevents confusion about outstanding payments.
Example: The total amount on this bill is “₹1200,” with the status marked as “Paid via Credit Card,” providing closure to the transaction.
To enhance the legitimacy of the document, the OP Bill typically includes the name of the staff member responsible for its preparation. This adds accountability and allows patients to direct any inquiries to the appropriate individual. Example:”Prepared by Ms. Priya Rao,” this bill assures professionalism and transparency in the billing process.
Modern OP Bills often incorporate QR codes, allowing patients to easily store, retrieve, or share their bills electronically. This integration facilitates seamless insurance claims, digital record keeping, and provides a hassle free experience for patients who prefer managing their healthcare digitally.

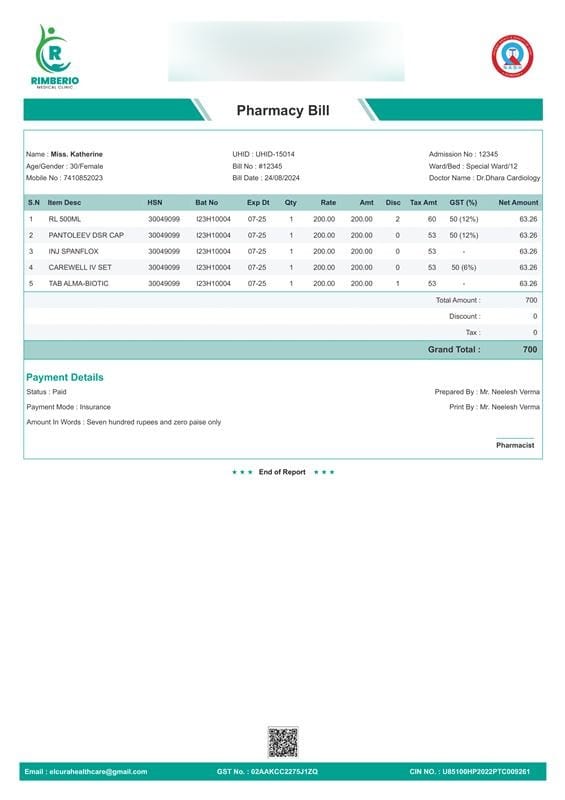
A pharmacy bill format is an essential document that details the medications or healthcare products dispensed to a patient. It provides a comprehensive breakdown of costs, taxes, and any discounts applied, while assisting with insurance claims and serves as a future reference.
Key Components of a Pharmacy Bill:
The patient’s personal details form the backbone of any medical pharmacy bill format . These include the patient’s full name, age, gender, contact information, and address. Such details are critical for establishing a clear connection between the patient and their respective medical records, ensuring accurate documentation and preventing any potential errors.
Example: In this case, the bill identifies the patient as “Miss. Katherine, 30 years old, residing in Cottonpet, Bangalore”
It is imperative for the bill to clearly outline the institution providing the medications. This includes the pharmacy’s or hospital’s name, physical address, contact numbers, and any relevant legal identifiers such as GST numbers. This not only establishes accountability but also ensures the patient knows exactly whom to contact for any billing or medication related inquiries.
Example: The bill is issued by “SRM Group of Hospitals, located at No:224, MH Lane, Teynampet, Chennai,” providing a solid point of reference for the patient.
When medications are prescribed during hospitalization, the attending doctor’s name and specialization, as well as the ward and bed details, must be recorded. This ties the pharmacy bill to the patient’s broader treatment plan, offering a transparent view of the medical professional responsible for the prescriptions.
Example: The attending physician for this case is “Dr. Dhara, a specialist in cardiology,” linking the prescribed medications to her expertise
Every bill must feature a unique bill number and the date of issue. These details are vital for tracking the transaction, whether for insurance claims, patient follow ups, or hospital accounting. The inclusion of a bill reference number ensures that any queries or future clarifications can be easily addressed by both the hospital and the patient.
Example: The bill was issued on “24/08/2024” with a unique reference number “#12345,” ensuring a clear trail for any financial reconciliation.
5. Itemized List of Medications and Products:
A transparent chemist bill format l will meticulously list all medications dispensed, along with essential details such as batch numbers, expiry dates, quantities, and individual pricing. Each item must be described clearly, leaving no ambiguity regarding what the patient has been charged for. This level of detail allows patients to understand the exact nature of the products received, aiding in both financial clarity and healthcare management.
Example: This bill details items such as “RL 500ML and PANTOLEEV DSR CAP,” each listed with its batch number, expiry date, and cost.
The breakdown of taxes, especially Goods and Services Tax (GST), is a crucial element in any bill. By clearly itemizing the applicable Central GST (CGST) and State GST (SGST), a well structured bill ensures that patients are aware of the government imposed charges. If any discounts are provided, whether for specific products or for broader reasons (such as insurance tie ups or senior citizen benefits), these must be reflected transparently to provide a clear net payable amount.
Example: In this particular bill, a 6% CGST and 6% SGST were applied, illustrating transparency in tax calculations.
A fundamental aspect of any bill is the clear articulation of the total amount due. It is essential for the patient to easily identify the gross amount, any deductions, and the final payable sum. Furthermore, indicating the payment status (whether paid or due) and the mode of payment used (cash, credit card, insurance, etc.) simplifies the transaction process, ensuring no confusion about outstanding payments or completed transactions.
Example: The total amount on this bill is “₹700,” and the status is marked as “Paid via Insurance,” providing closure to the transaction.
To further legitimize the document, the Pharmacy bill format typically includes the name of the billing staff responsible for preparing it. This adds an additional layer of accountability, ensuring that any future queries can be directed to the appropriate individual for resolution.
Example: “Prepared by Mr. Neelesh Verma,” this bill instills confidence in the professionalism and transparency of the process.
Modern pharmacy bills often include QR codes or digital links, making it easier for patients to store, retrieve, or share their bills electronically. This integration facilitates seamless insurance claims, digital record keeping, and promotes a hassle free experience for patients who prefer digital channels for managing their healthcare needs.
Hospital Bill Format: Comprehensive Breakdown
An inpatient bill formatis a detailed statement that outlines the costs associated with a patient’s stay in a hospital or healthcare facility. It includes charges for room and board, medical services, treatments, medications, and any additional procedures performed during the inpatient stay, providing a comprehensive overview of the patient’s healthcare expenses.
This section provides essential details about the patient, linking their identity to the medical and financial records of their stay. Accurately capturing this information ensures proper record keeping and billing.
This section details the hospital providing the care. It is critical for legal, financial, and communication purposes.
This section documents the dates and times related to the patient’s hospital stay and billing. It provides important context for the length of the stay and helps track financial transactions.
This section itemizes the charges associated with the patient’s room during their hospital stay. Different types of rooms have different rates, and the total cost depends on the duration of the stay.
This section provides a breakdown of specific medical services and procedures performed during the hospital stay. It includes charges for diagnostic tests, treatments, and any specialized procedures.
This section consolidates the overall inpatient bill format, including the total amount due, any advances paid, and the final balance.
This section tracks the payment methods used by the patient or their representatives and confirms the status of the payment.
This final section includes the credentials of the hospital staff who prepared and processed the bill, providing accountability and transparency
This detailed breakdown provides patients with full visibility of all financial transactions during their stay, ensuring transparency, and helping with future queries or insurance claims.

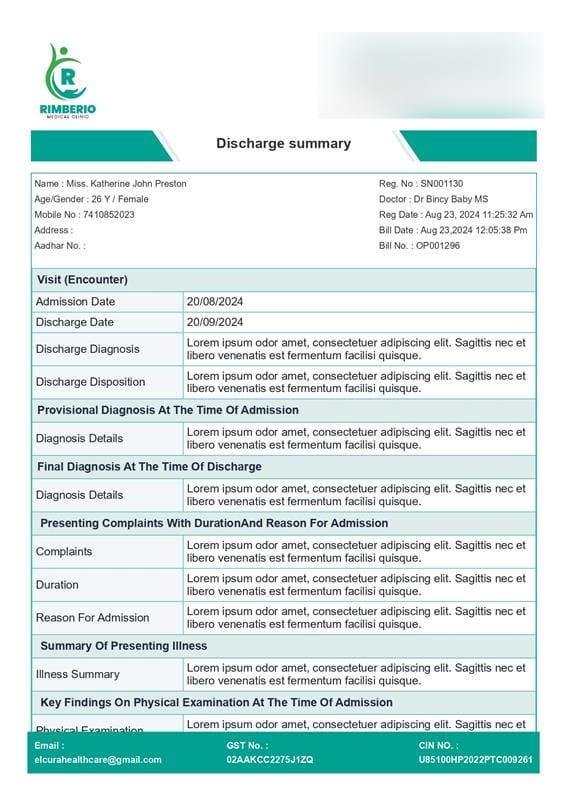
A discharge summary is a vital document provided upon a patient’s discharge from a healthcare facility. It details the patient’s medical journey during hospitalization and ensures continuity of care post-discharge. Ezovion has a facility to provide you customized format for hospital discharge summaries to reduce your time for charting a template for your patients to provide you with easy-to-use template.
1. Patient Information
The patient’s name, age, gender, and contact information provide the essential identification. Additionally, the admission number and registration number serve as unique identifiers linking the patient to medical and financial records throughout their stay.
Presenting Complaints: This section outlines the symptoms and concerns the patient reported during their first visit. For instance, a patient might report fever, headache, and body pain, which would guide the initial diagnostic approach.
The attending physician’s findings from the physical exam at the time of admission are recorded here. Key measurements, like vital signs (temperature, heart rate, blood pressure), are noted, along with any abnormalities found in organ systems such as the heart, lungs, or abdomen.
This section provides an overview of the patient’s health at the time of discharge. It may indicate whether the patient was discharged as fully recovered, in a stable condition requiring follow-up care, or transferred to another facility for specialized treatment. This status is important for setting expectations for post-discharge care.
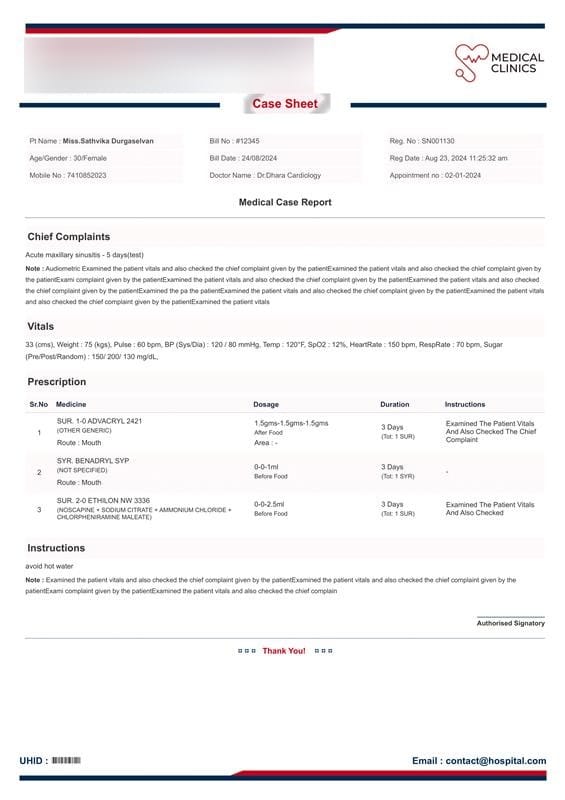
A case sheet summary provides a comprehensive record of the patient’s clinical journey during a medical visit or hospitalization. It includes vital details that serve as a reference for healthcare providers and ensures continuity of care for the patient.
1. Patient Information
The patient’s name, age, gender, and a unique patient number (e.g., RH22000003) are included to ensure accurate identification across medical records and for any follow-up consultations.
Name: Identifies the patient.
Age/Gender: Important for medical decision-making and treatment protocols.
Patient Number: This unique identifier links the patient to their health records, billing, and treatment details, ensuring continuity in care.
2. Attending Physician Information
The summary lists the doctor’s name, specialty, and the date and time of the consultation (e.g., Dr. Gola Swain, General Medicine, on 22-08-2024). This is crucial for tracking who administered care and provides transparency for accountability.
Doctor’s Name: Provides clarity on who treated the patient.
Specialty: Indicates the area of expertise relevant to the treatment.
Consultation Date and Time: A timestamp of when the patient received care.
3. Prescription Details
This section lists all the medications prescribed to the patient during the consultation. Each medication is thoroughly detailed with the following:
Medicine Name: Both the generic name and specific medicine prescribed (e.g., SUR. ABGEL REGULAR).
Dosage: Clearly defined dosing schedules (e.g., 3.0-0-3.0), indicating how many times per day the medication should be taken.
Duration: Specifies how long the patient should take the medication (e.g., 3 days).
Instructions: Additional usage instructions or precautions (if any) provided to the patient, ensuring the medication is used correctly and safely.
4. Injection or Procedural Treatmen
Any injection or other procedural treatments are documented here, including the following:
Injection Name: Lists injections (e.g., INJ. ADRENA INJ) prescribed during the consultation.
Dosage and Schedule: Specifies how often the injection should be administered (e.g., 0-0-1) and for how many days (e.g., 3 days).
Instructions: Additional instructions for injection administration, ensuring that the patient receives the correct dosage safely and on time.
5. Instructions and Follow-Up Care
In addition to prescribing medications, doctors often provide specific instructions for the patient’s post-consultation care. These instructions help the patient understand the care routine they must follow after leaving the healthcare facility.
Usage Instructions: Detailed guidelines on how to take medications, when to take them, and what precautions to follow. For example, the instructions may involve taking the medication with food, storing it at a particular temperature, or avoiding certain activities.
6. Consultation Date and Time
The consultation’s date and time (e.g., 22-08-2024, 6:50 PM) are recorded, which is useful for healthcare providers to track the timeline of treatment, especially for follow-up appointments. The timestamp ensures that future treatments or assessments can be compared against this baseline.
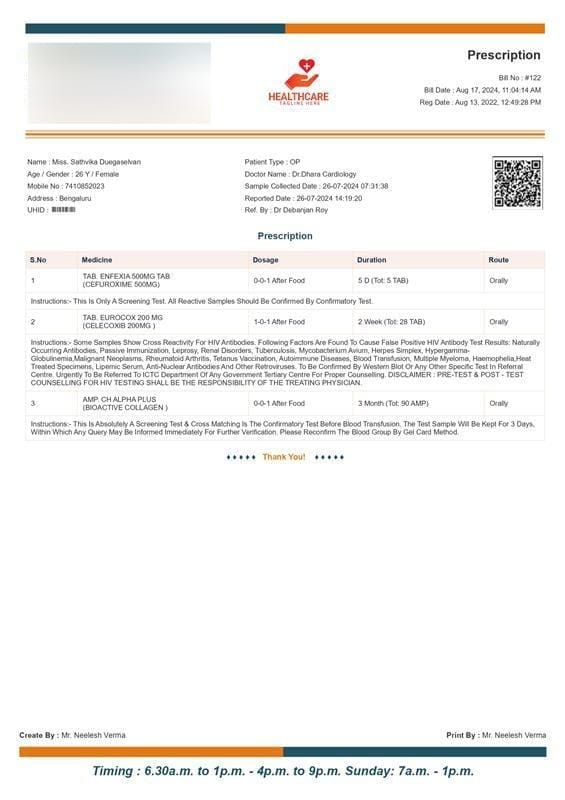

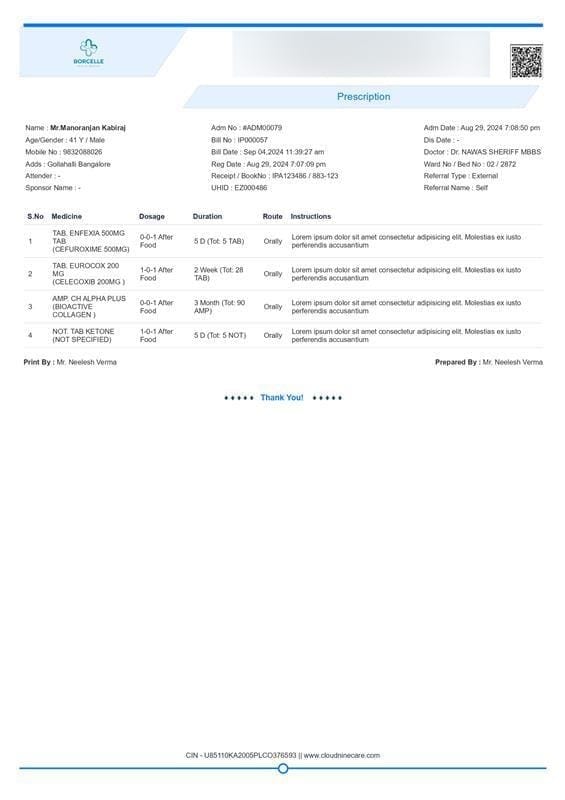
A doctor’s prescription sample is a critical document that provides detailed instructions for a patient’s medication regimen. It ensures clarity in the treatment process, guiding both patients and pharmacists on the correct medications and dosages. We have a set of well-curated formats of doctor’s prescriptions for easy edits and management of required information.
Key Components of a Prescription:
1. Patient Identification:
The prescription starts with the patient’s details, such as their full name, age, gender, and contact information. This information is key for ensuring the prescription is properly linked to the patient’s medical records and facilitates safe, personalized care.
Example: The prescription identifies the patient as “Miss Katherine, a 30-year-old female from Chennai.”
2. Healthcare Provider Information:
The healthcare provider’s name and relevant contact details must be included to establish accountability. This ensures that any questions regarding the treatment plan can be directed to the appropriate medical professional.
Example: The prescription is issued by “Dr. Dhara, a cardiologist from SRM Group of Hospitals, Chennai.”
3. Prescription Date and Reference Numbers:
Like an OP Bill, a prescription includes important administrative details such as the date of issuance and any registration or reference numbers for tracking.
Example: The prescription was issued on “24/08/2024” with a reference number “UHID-15014.”
4. Medication Details:
The core component of a prescription is the list of prescribed medications, along with dosage, frequency, and duration. This ensures clear communication regarding the treatment plan and helps prevent errors in medication administration.
Example: The prescription includes “TAB. ENFEXIA 500MG (Cefuroxime 500MG) to be taken 0-0-1 after food for 5 days.”
5. Dosage Instructions and Route:
Detailed dosage instructions for each medication, along with the route of administration (e.g., orally, injection), must be clearly specified to guide the patient and pharmacist.
Example: “TAB. EUROCOX 200 MG (Celecoxib 200MG) is to be taken 1-0-1 orally after food for 2 weeks.”
6. Special Instructions and Total Quantity:
Any special instructions regarding the medications, including total quantities and specific notes from the physician, are included to ensure full clarity. This can include dietary advice, side effects to watch for, or important reminders.
Example: “AMP. CH ALPHA PLUS (Bioactive Collagen) 0-0-1 after food for 3 months (Total: 90 AMP).”
7. Pharmacist Information:
For accountability, the name or signature of the pharmacist responsible for filling the prescription is often included. This ensures that any dispensing-related questions can be directed appropriately.
Example: The prescription was processed under the supervision of a registered pharmacist.
8. QR Code and Billing Information:
Modern prescriptions may also include QR codes for digital storage or tracking, making it easier for patients to manage their records. Additionally, GST or other billing information may be included, especially in the case of hospital-based prescriptions.
Example: The prescription includes a GST number and other billing details, ensuring financial transparency.
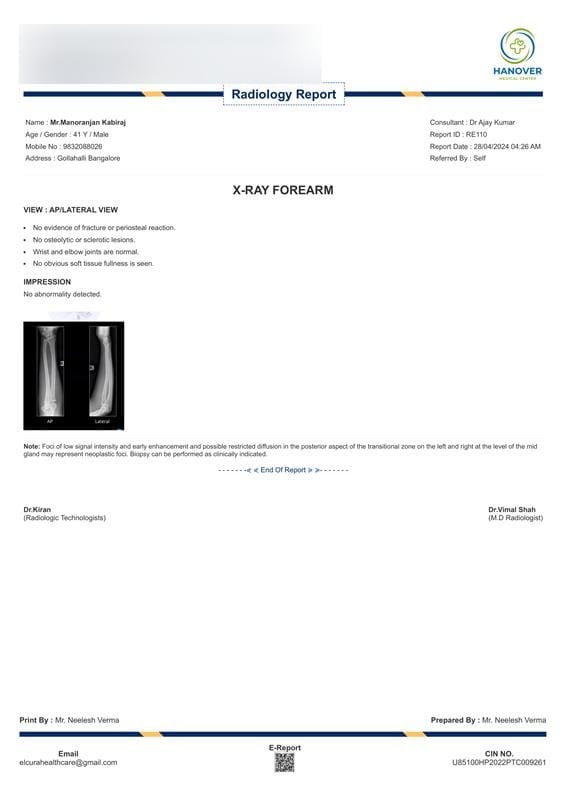
A radiology report is a formal document prepared by a radiologist that details the findings and interpretations of medical images like X-rays, MRIs, or CT scans. We provide radiology report samples for essential information guiding clinical decisions and facilitating communication between healthcare providers.
Key Components of a Radiology Report Template:
1. Patient Identification:
The report begins with the patient’s personal information, including their full name, age, gender, and contact details. This ensures that the report is correctly linked to the patient’s medical records.
Example: The radiology report identifies the patient as “Mr. Manoranjan Kabiraj, a 41-year-old male from Gollahalli, Bangalore.”
2. Healthcare Provider Information:
The report includes details of the healthcare provider or facility, ensuring accountability and enabling follow-up on the findings. This typically includes the name of the radiologist or technologist responsible for the report.
Example: The report was prepared at “Elcura Healthcare, Solan, Himachal Pradesh,” and the radiologist is “Dr. Vimal Shah.”
3. Report Date and Reference Numbers:
Administrative details such as the report date, bill number, and time of issuance are included for tracking and reference purposes.
Example: The report was issued on “28/04/2024 at 04:26 AM” with the bill number “#122.”
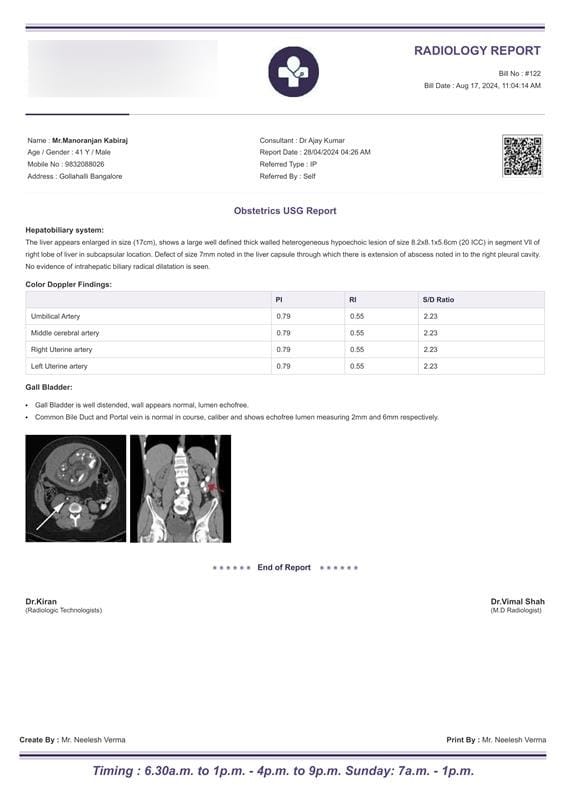
4. Imaging Technique and Findings:
This section provides details about the type of imaging performed (e.g., ultrasound, X-ray, CT scan) and outlines the findings based on the examination. This is the core part of the report, offering diagnostic information.
Example: The radiology report mentions “Obstetrics USG” and describes the findings in the hepatobiliary system, indicating “an enlarged liver with a heterogeneous lesion in segment VII of the right lobe.”
5. Detailed Analysis of Key Systems:
The report may break down the findings for specific organs or systems examined, providing a thorough analysis of each. This ensures that every abnormality or significant observation is clearly communicated.
Example: The liver is described in detail, noting “a lesion of size 8.2×8.1×5.6 cm” and a “defect in the liver capsule extending into the right pleural cavity.”
6. Color Doppler Findings (If Applicable):
If Doppler imaging is used, the report includes measurements of blood flow, such as the pulsatility index (PI), resistive index (RI), and systolic/diastolic (S/D) ratios, which help in assessing vascular conditions.
Example: The report lists Color Doppler findings for the umbilical artery, middle cerebral artery, and uterine arteries with consistent measurements.
7. Interpretation of Other Organs (If Applicable):
In some cases, the report may also examine other organs or systems, such as the gall bladder or bile ducts, ensuring comprehensive coverage of the imaging.
Example: The gall bladder is noted as “well-distended with a normal wall and echofree lumen.”
8. Radiologist’s Name and Signature:
The inclusion of the radiologist’s name and signature adds authority to the report, ensuring that a qualified professional has interpreted the results. This also provides a point of contact for any follow-up queries.
Example: The report is signed by “Dr. Vimal Shah, M.D. Radiologist.”
9. Technologist Information and Report Preparation Details:
Information about the radiologic technologist who conducted the scan and the details of report preparation (such as the time of creation) are included for completeness and accountability.
Example: The report was created and printed by “Mr. Neelesh Verma” with timing details mentioned for operational hours.

Lab reports are essential documents that should be in a proper format. All the essential details required for patient reference regarding the respective test should be maintained carefully on the template. Ezovion has neatly designed lab report templates that ensure to portray all the required details of the test along with control values with hospital and technician information.
Patient Identification
Patient details ensure the report is assigned to the correct individual and provide essential demographic information for accurate interpretation. Data like patient name, age, gender, and contact details ensure streamlined communication and precise test result analysis. Example:
Hospital Information
The hospital’s name, address, and contact details establish the source of the report, ensuring authenticity and enabling direct contact for clarifications.
Example-
Physician and Hospitalization Details
Details like the physician’s name, department, and report date help link the test results to the prescribing doctor, ensuring timely follow-ups.
Example: Physician: Dr. Abhirami Palanisamy, Department: General Medicines, Report Date: 30-12-2024 12:48:23.
Investigation Details
A clear list of tests conducted provides transparency and simplifies result interpretation. This includes test categories and names
Examples: Haematology, WBC, RBC, potassium, blood glucose, and uric acid.
Results
Test outcomes and their values, units, and normal reference ranges offer actionable insights into the patient’s health.
Example:
Test | Test Value | Control Range | Unit |
WBC (White Blood Cell Count)
| 7,500 | 4,500 – 11,000 | UI/mL |
RBC (Red Blood Cell Count)
| 4.8 million | 4.2 – 5.9 million | UI/mL |
Potassium
| 4.2 | 3.5 – 5.1 | UI/mL |
Blood Glucose
| 92 | 70 – 99 | UI/mL |
Uric Acid
| 5.6 | 3.4 – 7.2 (men) 2.4 – 6.0 (women)
| UI/mL |
Processing and Verification Details
Details of the lab technician and in-charge ensure accountability and quality assurance in report preparation.
Example: Technician: John Doe, In-Charge: Jane Smith.
