Let’s be honest, dealing with medical billing can feel like trying to solve a puzzle blindfolded. You’ve got patients to care for, paperwork piling up, and then… those dreaded claim denials. It’s frustrating, time-consuming, and can hit your practice’s bottom line. You’re not alone, though. According to a study by the Medical Group Management Association (MGMA), the average claim denial rate can be anywhere from 5-10%, and some practices see even higher numbers. That’s a lot of lost revenue! You pour your heart into providing excellent care, so why should administrative headaches steal your hard-earned money? That’s where medical billing software comes in. It’s like having a super-efficient assistant who knows all the ins and outs of billing, helping you navigate the complexities and get paid faster. Let’s dive into how this software can become your best friend in reducing claim denials and bringing peace of mind to your practice.
Automated Coding with Medical Billing Software: Saying Goodbye to Costly Errors
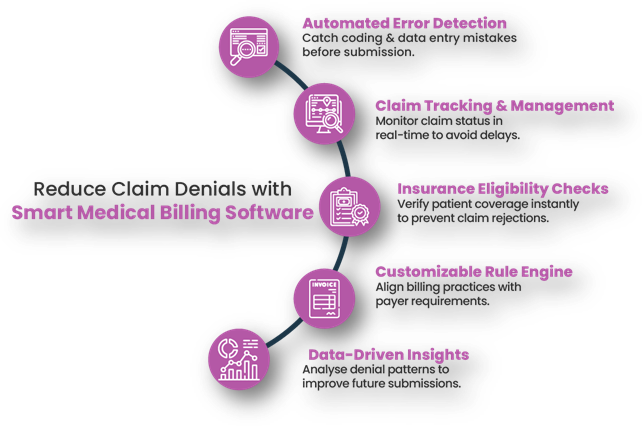
We all know how tricky medical coding can be. One tiny mistake, a misplaced decimal, or using the wrong code, and bam! Denial. It’s easy to see why coding errors are a major cause of claim denials. But imagine a system that automatically checks your codes against the latest guidelines and regulations. That’s exactly what medical billing software does. It uses advanced algorithms to ensure accuracy, reducing the risk of human error. It’s like having a coding expert on your team, 24/7. This kind of automation isn’t just about accuracy; it’s about freeing up your staff to focus on more important things, like patient care. Think about it: less time spent on tedious coding means more time for your patients, and that’s what truly matters.
Automated coding within medical billing software simplifies the coding process by integrating up-to-date coding databases. It can automatically suggest codes based on the entered patient information, and it flags potential errors before claims are submitted. This helps to prevent common mistakes like using outdated codes or missing required modifiers. According to the American Academy of Professional Coders (AAPC), accurate coding is crucial for reimbursement. By automating this process, practices can significantly reduce the number of errors that lead to denials, ensuring that claims are clean and compliant from the outset. This not only speeds up the payment cycle but also reduces the stress and frustration associated with manual coding and subsequent denials.
Real-Time Eligibility Verification: Knowing Before You Go
Imagine submitting a claim, only to find out the patient’s insurance had lapsed weeks ago. Talk about a waste of time! Real-time eligibility verification is a game-changer. Medical billing software can instantly check a patient’s insurance status, ensuring they’re covered before you provide services. This feature alone can drastically reduce denials caused by ineligible patients. It’s like having a crystal ball that lets you see potential problems before they happen. This not only saves you money but also helps you provide a smoother experience for your patients. No one likes surprises when it comes to their healthcare costs.
Real-time eligibility verification allows for immediate checks against payer databases. This ensures that the patient’s insurance is active and that the services provided are covered under their plan. Medical billing software can perform these checks in seconds, providing instant feedback to your staff. This prevents the submission of claims for services that are not covered, which is a major cause of denials. By verifying eligibility upfront, practices can also improve patient communication, as they can inform patients about their coverage and potential out-of-pocket costs before providing care. This transparency enhances patient satisfaction and reduces the likelihood of billing disputes later.
Managed Claim Submission: Getting It Right the First Time
Let’s face it, submitting claims manually can be a real headache. You have to fill out forms, double-check everything, and hope you haven’t missed anything. Medical billing software streamlines the entire process, making it faster and more efficient. It can automatically generate and submit claims electronically, reducing the risk of errors and delays. It’s like having a well-oiled machine that handles all the paperwork for you. This means fewer denials, faster payments, and more time to focus on what you do best: caring for your patients.
Streamlined claim submission in medical billing software involves the electronic transmission of claims directly to payers. This eliminates the need for manual data entry and paper-based submissions, which are prone to errors. The software can automatically format claims according to payer requirements, ensuring that all necessary information is included. It also tracks the status of submitted claims, providing real-time updates and alerts for any issues. This proactive approach helps to identify and resolve potential problems before they lead to denials. By automating the submission process, practices can improve their first-pass claim acceptance rate, leading to faster reimbursement and a more efficient revenue cycle.
Why Medical Billing Software is Essential
Managing billing manually in healthcare can lead to serious inefficiencies and revenue losses. Without a proper system, clinics and hospitals may struggle with accuracy, compliance, and timely reimbursements, affecting both patient care and financial stability.
Gaps Without Medical Billing Software:
- Billing Errors & Revenue Loss: Manual entry increases the risk of mistakes, leading to claim denials and lost revenue.
- Delayed Payments: Slow processing times cause delayed reimbursements and cash flow issues.
- Compliance Risks: Difficulty in keeping up with changing healthcare regulations (like CPT or ICD codes) can result in penalties.
- Lack of Tracking & Reporting: Limited visibility into payment status, outstanding claims, and financial performance.
- Poor Patient Experience: Billing inaccuracies and delayed invoices frustrate patients and erode trust.
- Inefficient Claim Management: Manual handling makes tracking, submitting, and resubmitting claims time-consuming.
- Resource Overload: Administrative staff waste valuable time on paperwork instead of patient care.
Let’s have a look-
A recent study by Pristyn Care has revealed that more than half of the patients in India face delays in their discharge from hospitals due to the time taken to process medical insurance claims. This delay can lead to increased stress and anxiety for patients and their families.
Key findings from the study include:
- Hospital Administrative Processes: Over 40% of delays are due to cumbersome and time-consuming hospital administrative processes.
- Coordination Issues: Around 25% of delays result from a lack of coordination between hospitals and insurance providers.
- Complex Documentation: The complexity of the required documentation significantly contributes to delays.
- Customer Support Difficulties: Nearly 40% of respondents reported difficulties with customer support during the claims process.
These findings highlight the need for improved efficiency and better coordination in the medical insurance claims process to reduce discharge delays and alleviate stress for patients and their families.
Tracking and Reporting: Spotting Problems Before They Grow
Imagine being able to see exactly where your claim denials are coming from. That’s the power of tracking and reporting. Medical billing software provides detailed reports on your claim submissions and denials, allowing you to identify trends and patterns. You can see which codes are causing the most problems, which payers are denying claims, and where your staff might need additional training. It’s like having a detailed map that shows you exactly where you need to improve. By spotting problems early, you can take steps to fix them and prevent future denials.
Tracking and reporting features in medical billing software provide valuable insights into the practice’s billing performance. The software can generate reports on key metrics such as denial rates, average payment times, and claim status. These reports can be customized to focus on specific areas of concern, such as particular payers or service codes. By analysing these reports, practices can identify the root causes of denials and implement corrective actions. For example, if a particular code is consistently being denied, the practice can review its documentation and coding practices to ensure accuracy. This data-driven approach allows for continuous improvement and helps to prevent recurring denials.
In the end, medical billing software isn’t just a tool; it’s a partner in your practice’s success. It takes the stress out of billing, reduces claim denials, and helps you get paid faster. So, if you’re tired of dealing with claim denials, consider investing in medical billing software. It might just be the best decision you make for your practice.
Optimize your billing, reduce denials, and get paid faster with Ezovion’s Medical Software Solutions!





