
In the fast-paced world of healthcare, even a small oversight in medication administration can lead to serious consequences. Medication Safety is no longer a side note—it has become a central priority. Clinical practices that integrate structured protocols, such as the WHO 5 Moments for medication safety, can significantly improve efficiency, reduce errors, and enhance patient outcomes.
The WHO 5 Moments offers a globally recognized approach that ensures safety at every touchpoint in the medication-use process. By incorporating these actionable steps, hospitals and clinics can embed safety into the core of every patient interaction.
Understanding the WHO’s 5 Moments for Medication Safety
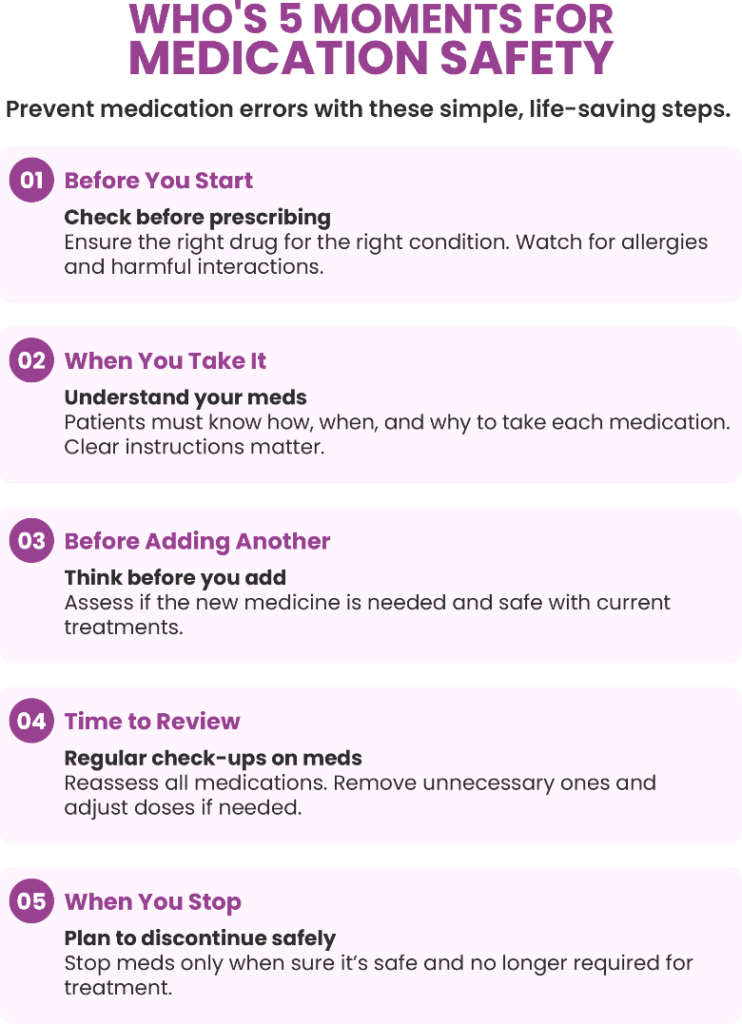
The WHO’s 5 Moments for Medication Safety provide a structured approach to identify key points where interventions can prevent medication errors. These moments are:
• Starting a Medication: Before initiating any medication, healthcare professionals should ensure the appropriateness of the drug, considering the patient’s condition, potential allergies, and possible interactions with other medications.
• Taking My Medication: This moment emphasizes the importance of patients understanding how and when to take their medications correctly. Clear instructions and education can empower patients to adhere to their treatment regimens effectively.
• Adding a Medication: When introducing a new medication, it’s crucial to assess its necessity and compatibility with existing treatments. This step helps in preventing adverse drug interactions and ensures the added medication contributes positively to the patient’s health.
• Reviewing My Medication: Regularly reviewing all medications a patient is taking allows for the identification of redundant or unnecessary drugs, dosage adjustments, and monitoring for side effects.
• Stopping My Medication: Discontinuing a medication should be a deliberate process, ensuring that stopping the drug won’t negatively impact the patient’s health and that it’s no longer needed.
Implementing these moments in clinical practice fosters a culture of safety and encourages proactive measures to prevent medication errors.
Challenges in Implementing the 5 Moments in Healthcare
While the WHO’s 5 Moments provide a clear framework, integrating them into daily clinical routines can present challenges:
• Time Constraints: Healthcare professionals often operate under tight schedules, making it difficult to thoroughly assess each moment for every patient.
• Lack of Awareness: Not all staff may be familiar with the 5 Moments, leading to inconsistent application across departments.
• Communication Gaps: Effective medication safety relies on clear communication among healthcare teams, which can be hindered by hierarchical structures or inadequate information systems.
• Addressing these challenges requires a multifaceted approach, including staff education, streamlined processes, and supportive technologies.
Integrating WHO’s 5 Moments into Electronic Health Records (EHR)
Modern clinical practice thrives on digitization. Integrating the WHO 5 Moments into EHR systems offers real-time prompts, validation checks, and seamless access to patient medication histories.
• Digitized Prescribing and Dispensing
EHR systems equipped with AI modules can automatically flag high-risk medications, check for drug interactions, and ensure prescribers adhere to the first and second WHO Moments. These tools ensure best practices for medication safety in hospitals are followed with minimal room for error.
• Barcode Scanning for Administration
At the administration stage, EHR integration allows clinicians to scan patient IDs and medications, automatically cross-checking them with the order. This step enforces medication safety and aligns perfectly with the third WHO Moment.
• Monitoring and Reconciliation Dashboards
EHRs offer smart dashboards for continuous monitoring, lab result integration, and reconciliation across departments. This digitization supports effective application of the fourth and fifth WHO Moments and reinforces staff accountability throughout the process.
Research Work on Integrating EHR into WHO’s Moments
Integrating the World Health Organization’s (WHO) into Electronic Health Records (EHRs) can significantly enhance infection control in hospitals and clinics. This integration facilitates real-time monitoring, improves compliance, and reduces healthcare-associated infections (HAIs). Below is a summary of relevant studies and data supporting this integration.
Comparative Compliance Rates: WHO 5 Moments vs. Entry/Exit Methods
| S.NO | Hand Hygiene Method | Compliance Rate | Study Details |
| 1 | WHO 5 Moments | 73.8% | Observed over 5 months in ICU and surgical/medical wards. |
| 2 | Entry/Exit | 59.5% | Same study as above. |
| 3 | Self-reported (All Moments) | 82.4% | Compared to 23.2% observed compliance. |
The study comparing three approaches showed that the WHO 5 Moments achieved a 73.8% compliance rate in ICU and surgical wards over five months. In contrast, the Entry/Exit method, which tracks hygiene only at room entry and exit, recorded a lower compliance of 59.5%, potentially missing key hygiene moments like before aseptic tasks. Self-reported compliance was the highest at 82.4%, but actual observed compliance was much lower, around 23.2%, highlighting the inaccuracy of self-reporting.
Incorporating WHO’s 5 Moments into EHR systems can overcome these challenges by providing real-time alerts, data collection, and automated tracking. This helps standardize practices, enables targeted training, and fosters a stronger safety culture. Ultimately, this integration not only improves infection control but also elevates care quality, making it a smart move for hospitals and clinics aiming for better outcomes and accountability.
Compliance by Individual Moments
| S.No | Moment | Observed Compliance | Notes |
| 1 | Moment 1: Before patient contact | 8.21% | Lowest compliance observed. |
| 2 | Moment 2: Before aseptic task | 20% (nurses & allied HCPs), 0% (medical) | Significant disparity among professions. |
| 3 | Moment 3: After body fluid exposure | 33.93% | Highest compliance among all moments. |
| 4 | Moment 4: After touching patient | 22.71% | Moderate compliance. |
| 5 | Moment 5: After touching patient surroundings | 18.95% | Lower compliance, especially among medical staff. |
The table “Compliance by Individual Moments” provides a closer look at how well healthcare professionals adhere to each of the WHO’s 5 Moments for Hand Hygiene. It reveals a stark contrast in observed compliance across the five defined moments, offering critical insights into behavior patterns and areas needing improvement.
Moment 1 (Before patient contact) shows the lowest compliance at just 8.21%, indicating a significant gap in initiating hand hygiene before interacting with patients—a key moment for preventing germ transmission.
Moment 2 (Before aseptic task) further highlights professional disparities, with 20% compliance among nurses and allied health professionals but 0% among medical staff. This suggests that more training and monitoring may be needed specifically for physicians during clinical procedures.
Moment 3 (After body fluid exposure) reports the highest compliance at 33.93%, likely due to an instinctive reaction to perceived contamination risk. However, despite being the best, even this rate is alarmingly low considering the critical nature of this moment.
Moment 4 (After touching a patient) records a moderate compliance rate of 22.71%, while Moment 5 (After touching patient surroundings) drops again to 18.95%, especially low among medical staff. These figures show that indirect contact is underestimated as a transmission risk.
Overall, the data underscores the need for targeted interventions, especially for Moments 1, 2, and 5. Integrating such granular compliance tracking into Electronic Health Records (EHRs) can prompt timely hygiene actions, generate role-specific insights, and support behavior change, thus fostering a safer clinical environment.
Engaging Patients in Medication Safety Using WHO’s 5 Moments
Patient involvement remains a game-changing element of safe medication use. When patients understand their treatment, they become active participants rather than passive recipients. Recent studies by the International Journal for Quality in Health Care show that patients who receive medication counseling experience 45% fewer adverse drug events.
• Encourage Open Communication
Clinicians should explain prescriptions clearly and encourage patients to ask questions. Involving patients during prescribing, dispensing, and administration stages aligns with the WHO 5 Moments model and improves compliance.
• Use of Digital Patient Portals
Through digital platforms, patients can view their medications, receive dosage alerts, and access educational resources. These tools create a transparent channel between providers and patients, reinforcing the importance of medication safety at every step.
• Include Caregivers and Family
Involving caregivers during medication reconciliation ensures continuity and reduces the chance of forgotten or duplicated drugs, especially in elderly care. Training programs can also be extended to family members to strengthen the model further.
Embracing the WHO’s 5 Moments for a Safer Clinical Practice
Integrating the WHO’s 5 Moments for Medication Safety into clinical practice offers a structured approach to minimizing medication errors and enhancing patient care. By addressing implementation challenges through education, technology, and patient engagement, healthcare organizations can foster a culture of safety and efficiency. Embracing these practices not only improves outcomes but also reinforces the commitment to delivering high-quality, patient-centered care.





