
Healthcare-associated infections (HAIs) pose a significant threat to patients, healthcare workers, and the broader health system. These infections not only lead to increased morbidity and mortality rates but also extend hospital stays and inflate healthcare costs. With the growing concerns over life-threatening infections like severe acute respiratory syndrome (SARS) and the re-emergence of diseases such as tuberculosis and plague, the need for robust infection control programs has never been more critical. Implementing efficient infection control measures helps safeguard both patients and healthcare workers, ensuring that hospitals remain safe environments for healing.
The Importance of Infection Control Programs
An effective infection control program is designed to restrict the spread of infections within healthcare settings. When properly implemented, these programs can significantly reduce infection rates among patients and healthcare staff, thereby decreasing patient morbidity and mortality. Additionally, they contribute to shorter hospital stays and lower costs related to hospitalization. Central to these programs is the application of evidence-based practices to prevent and manage infections.
These programs are not static; they need to evolve in response to emerging health threats and new research. With the rapid changes in the global health landscape, hospitals must continuously update their strategies to remain effective.
Key Components of an Infection Control Program
Infection control programs consist of several essential components, each contributing to a comprehensive strategy to prevent and manage infections in healthcare settings. The following are the key elements of a control program:
- Basic Measures for Infection Control:
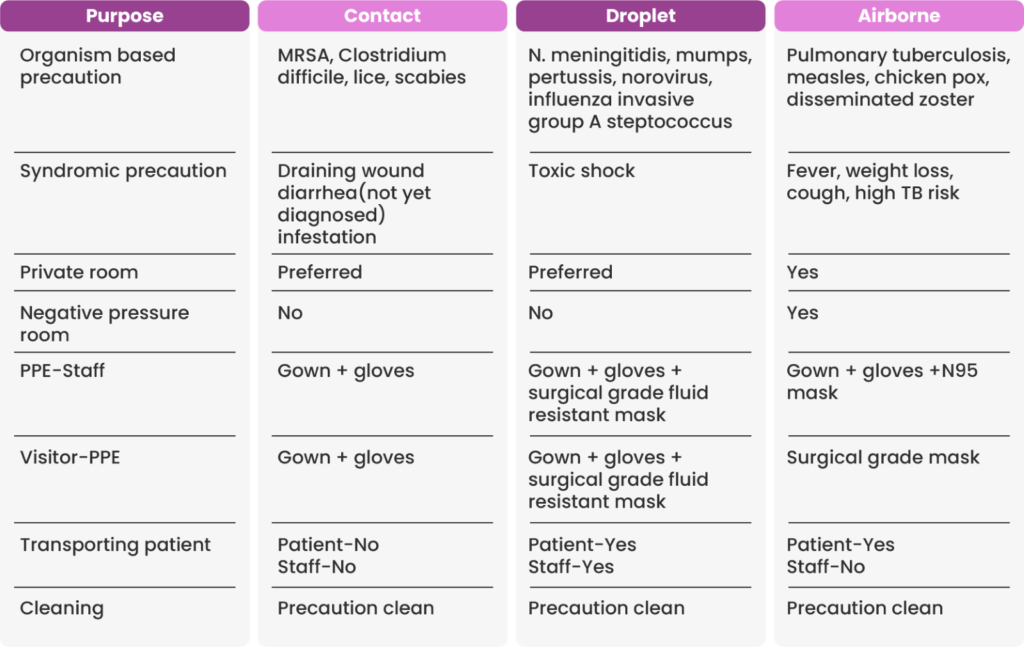
These include standard precautions, such as hand hygiene, and additional precautions like contact, droplet, and airborne precautions, which are implemented depending on the transmission risk.
- Education and Training of Healthcare Workers:
Ongoing education ensures that healthcare workers have the latest knowledge and skills to implement infection control measures effectively.
- Protection of Healthcare Workers:
This includes providing personal protective equipment (PPE) and ensuring healthcare workers are vaccinated and trained to avoid infection exposure.
- Identification of Hazards and Risk Minimization:
Regular assessments to identify potential risks and implement strategies to minimize them are essential to an infection control program.
- Aseptic Techniques:
The use of aseptic techniques during medical procedures minimizes the risk of introducing infections to patients.
- Management of Medical Devices and Instruments:
The use of single-use devices, as well as the proper reprocessing of reusable instruments, helps reduce infection risks.
- Antibiotic Stewardship and Management of Blood/Body Fluid Exposure:
Proper antibiotic usage, along with the careful handling of blood and blood products, is essential to infection prevention.
- Surveillance:
Continuous monitoring for infections within the healthcare facility allows for timely identification and response to outbreaks.
- Outbreak Investigation:
Investigating infection outbreaks and implementing corrective measures help prevent future occurrences.
- Incident Monitoring:
Documenting and analysing infection control incidents ensures that lessons are learned and improvements are made.
Universal Precautions: Protecting Healthcare Workers from Infections
Universal precautions are a fundamental aspect of contamination control. These guidelines are designed to protect healthcare workers from exposure to bloodborne infections such as HIV, hepatitis B, and hepatitis C. The concept behind universal precautions is simple: every patient should be treated as though they are potentially infectious. This assumption ensures that healthcare workers remain vigilant and consistently apply contamination control measures.
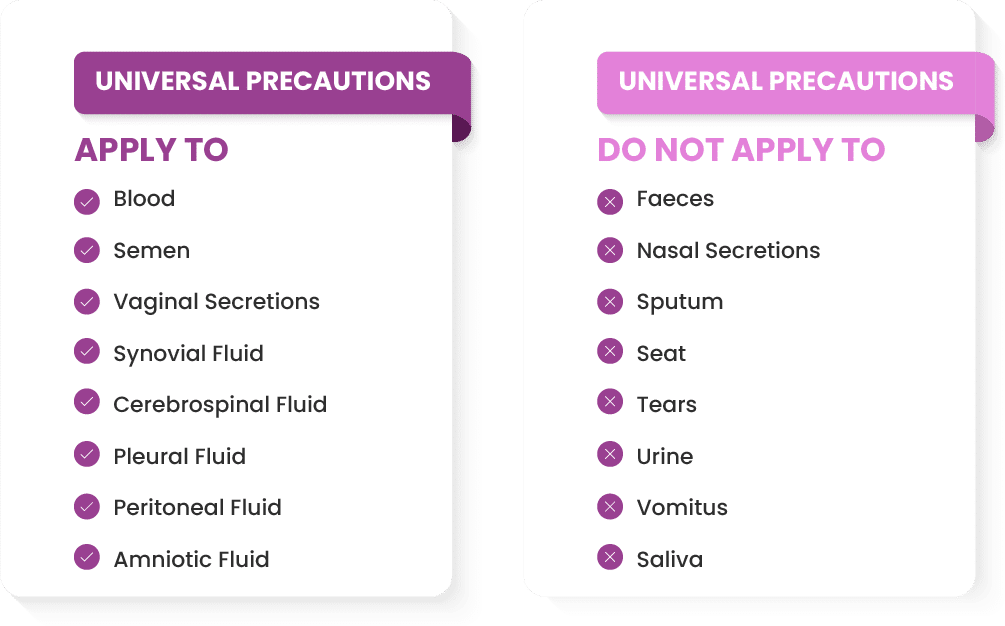
The core elements of universal precautions include:
- Personal Protective Equipment (PPE):
Gloves, gowns, masks, and goggles are essential barriers that protect healthcare workers from direct exposure to infectious materials. PPE creates a physical barrier between the worker’s skin and mucous membranes and potentially infectious blood or body fluids.
- Engineering Controls:
These measures involve modifying the healthcare environment to reduce the risk of infection. Examples include the use of sharps disposal containers and biological safety cabinets.
- Work Practice Controls:
Changing the way tasks are performed can also reduce the likelihood of infection. For example, proper handwashing, the correct handling of sharps, and appropriate disposal of biological waste are all crucial work practice controls.
Main Objectives of Infection Control Programs
The primary goal of infection control programs is to prevent the transmission of infections within healthcare settings. More specifically, these programs aim to:
- Provide healthcare workers with the facilities, equipment, and procedures necessary to implement contamination control measures effectively.
- Ensure the safe cleaning, disinfecting, and reprocessing of reusable medical equipment.
- Manage waste and ensure its safe disposal to prevent environmental contamination.
- Protect healthcare workers from infections transmitted during patient care.
- Prevent healthcare-associated infections (HAIs) in patients through effective contamination control practices.
- Implement specific contamination control measures in unique situations, such as during outbreaks or in high-risk environments.
Infection Control in Special Situations
Infection control programs must also address special circumstances that may arise in healthcare settings. For example, during an outbreak, hospitals must act quickly to contain the infection and prevent further transmission. Surveillance and rapid response teams play a critical role in identifying and managing these situations. Additionally, contamination control measures need to be adaptable to different areas of the hospital, such as intensive care units (ICUs), surgical theaters, and outpatient clinics, where the risk of infection may vary.
Conclusion
Infection control is a critical component of healthcare management. Effective infection control programs help prevent healthcare-associated infections, protect healthcare workers, and reduce healthcare costs. By focusing on key components such as education, aseptic techniques, and surveillance, hospitals can create safer environments for both patients and staff. Universal precautions, personal protective equipment, and work practice controls are all essential elements in protecting healthcare workers from infectious diseases. Implementing these measures ensures that hospitals can continue to provide high-quality care while minimizing the risks associated with infections.
Source-





