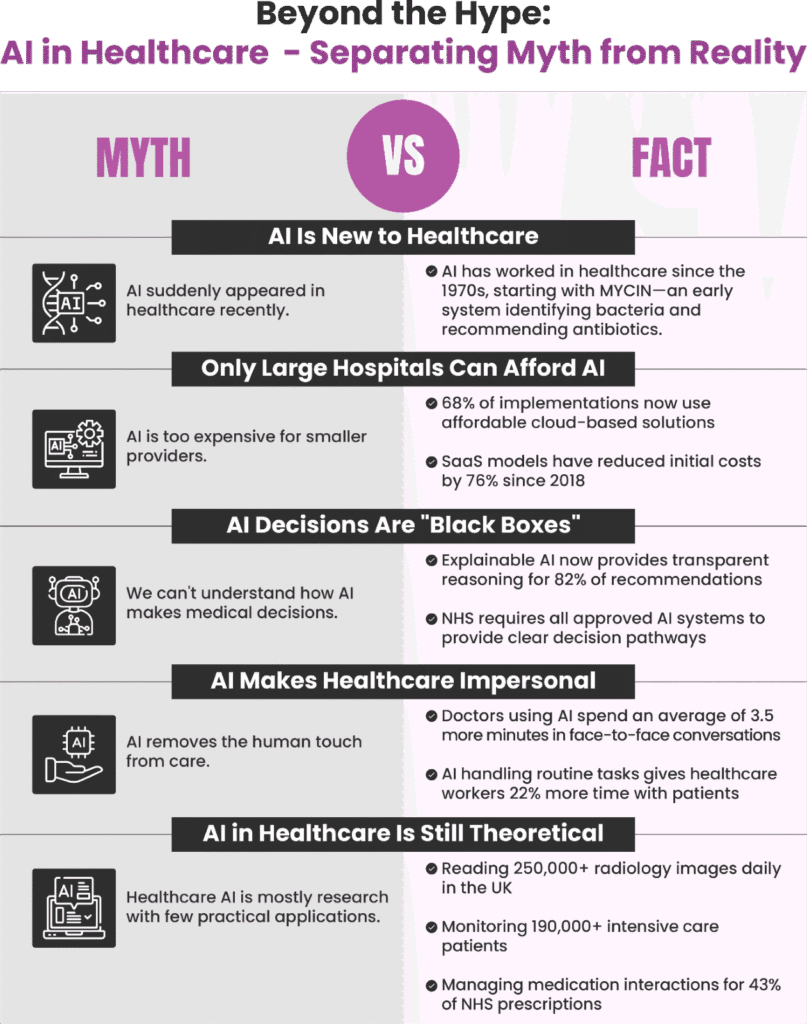
Imagine walking into a doctor’s office where a computer has already reviewed your medical history, predicted potential health issues, and suggested treatment options all before you’ve even sat down. This isn’t science fiction; it’s the emerging reality of AI in healthcare. From chatbots handling initial patient inquiries to algorithms detecting cancer in scans more accurately than trained professionals, AI is transforming how we approach medicine. Yet, for every breakthrough headline, there’s a matching concern about privacy, accuracy, and the future role of human healthcare providers.
The intersection of cutting-edge technology and personal health naturally breeds both excitement and anxiety. As AI becomes increasingly embedded in our healthcare systems, understanding the line between hype and reality has never been more important. This article aims to separate myth from fact, helping you navigate the promises and pitfalls of AI in the medical world with clarity and confidence.
Myth: AI Will Replace Doctors and Nurses
What people believe:
- Robots will eventually take over all medical procedures
- Human healthcare workers will become obsolete
- AI can make all medical decisions independently
- Hospitals of the future will be run entirely by machines
The reality: AI is designed to assist healthcare professionals, not replace them. Think of AI as a powerful tool in a doctor’s kit, like a stethoscope or X-ray machine, rather than a substitute for the doctors themselves. According to a 2023 report by the NHS, AI tools have helped increase diagnostic efficiency by 30% whilst reducing clinician workload, but patient satisfaction remained highest when AI was used alongside human care providers rather than instead of them.
What’s actually happening is a partnership between human expertise and technological capability. While AI excels at processing vast amounts of data and identifying patterns, it lacks the emotional intelligence, ethical judgment, and contextual understanding that human healthcare providers bring to patient care. The most effective healthcare systems of the future will likely combine the analytical power of AI with the compassion and intuition of human professionals.
Table 1: AI’s Impact on the Healthcare Workforce
| Current Concern | Emerging Reality |
| Job displacement fears | Creation of new specialised roles like AI implementation specialists |
| Changes to existing workflows | Reduction of administrative burden, allowing focus on patient care |
| Training requirements | Development of AI literacy programs for healthcare professionals |
Myth: AI Diagnoses Are Always Accurate
What people believe:
- AI systems never make mistakes
- Machine learning always produces perfect results
- Algorithms are free from the biases that affect human judgment
- AI diagnosis is universally superior to human diagnosis
The reality: AI systems are powerful but imperfect. They’re only as good as the data they’re trained on, and if that data contains biases or gaps, the AI will reflect those limitations. A study published in the British Medical Journal found that while some AI diagnostic tools achieved 90% accuracy in controlled settings, performance dropped to 75-80% when deployed in diverse real-world environments.
It’s also worth noting that AI systems typically specialise in narrow tasks rather than demonstrating the broad understanding of human physicians. For example, an algorithm might excel at identifying a specific type of skin cancer from images but struggle with conditions it wasn’t explicitly trained to recognise. This is why most medical AI is designed to support human decision-making rather than operate independently. The most promising approach seems to be a collaborative model where AI helps identify potential issues that a healthcare professional then evaluates in context.
Table 2: AI Diagnostic Support Across Medical Fields
| Medical Field | AI Capabilities | Human Specialist Role | Complementary Relationship |
| Dermatology | Pattern recognition in skin lesions | Clinical context and patient history | AI flags concerning images for specialist review |
| Radiology | Detection of subtle abnormalities in scans | Interpretation based on medical history | AI serves as a “second pair of eyes” for radiologists |
| Ophthalmology | Screening for retinal conditions | Treatment decisions and patient management | AI enables wider population screening by pre-filtering images |
Myth: AI in Healthcare Is Just a Passing Trend
What people believe:
- AI is merely the latest healthcare fad
- The technology isn’t mature enough for serious medical application
- Previous technological promises in healthcare haven’t delivered
- The industry will eventually revert to traditional methods
The reality: Far from being a temporary trend, AI represents a fundamental shift in healthcare delivery. Global investment in healthcare AI reached £10.3 billion in 2023, with projected annual growth of 37% through 2028, according to Healthcare UK. The NHS’s Long-Term Plan explicitly incorporates AI solutions as central to meeting future healthcare demands.
The technology has already made measurable impacts across multiple healthcare domains:
- Administrative efficiency: AI-powered systems have reduced documentation time by up to 70%
- Diagnostic support: Algorithm-assisted image analysis has improved early detection rates for certain cancers by 26%
- Treatment planning: AI tools have helped optimise medication dosing, reducing adverse drug events by 35% in pilot programmes
Healthcare organisations are increasingly integrating AI into their core operations rather than treating it as an experimental add-on. These aren’t speculative applications but working solutions already delivering results in healthcare systems worldwide.
Table 3: Patient Acceptance of AI in Healthcare
| AI Application | Level of Patient Acceptance | Key Factor Influencing Acceptance |
| Administrative tasks | High acceptance | Minimal perceived risk, clear efficiency benefits |
| Appointment scheduling | Widely accepted | Convenience and 24/7 availability |
| Diagnostic support (with doctor oversight) | Moderate acceptance | Reassurance of human verification |
| Autonomous diagnosis or treatment | Low acceptance | Concerns about accountability and human judgment |
Myth: AI in Healthcare Threatens Patient Privacy
What people believe:
- AI systems automatically share personal health information
- Patient data used to train AI is easily identifiable
- Privacy regulations can’t keep pace with AI development
- Medical AI requires sacrificing confidentiality
The reality: While data security is a legitimate concern with any digital technology, responsible AI development includes robust privacy protections. In the UK, AI healthcare applications must comply with the Data Protection Act 2018 and the NHS Data Security and Protection Toolkit standards, providing multiple layers of patient protection.
Many AI systems now use techniques like federated learning, where algorithms are trained across multiple data locations without centralising sensitive information. This allows the AI to learn patterns without directly accessing identifiable patient records. Additionally, anonymisation techniques continue to advance, making it increasingly possible to use health data for AI training whilst protecting individual privacy.
Rather than viewing AI and privacy as opposing forces, healthcare organisations are finding ways to harness AI’s benefits while enhancing data protection. With proper governance frameworks, AI can actually improve security by detecting unusual access patterns and potential data breaches more effectively than traditional monitoring.
Who Is Leading AI in Healthcare?
Major players include:
- Academic medical centres like Oxford University Hospitals NHS Trust
- Technology giants, including Google Health, Microsoft, and IBM
- Specialised AI healthcare startups such as Babylon Health and DeepMind Health
- Government entities like the NHS AI Lab
The landscape: The UK has emerged as a significant player in healthcare AI innovation, with London alone hosting over 100 AI health startups. The NHS AI Lab, launched in 2019 with £250 million in funding, coordinates national efforts to accelerate safe AI adoption across the healthcare system.
International collaboration is increasingly common, with cross-border research partnerships developing solutions for global health challenges. Meanwhile, traditional healthcare providers are forming strategic alliances with technology companies to combine medical expertise with AI capabilities.
Competition remains fierce, but there’s growing recognition that addressing healthcare’s most pressing challenges requires cooperation alongside innovation. Leading organisations are increasingly sharing datasets, research findings, and best practices to accelerate progress in the field.
How Does AI Reduce Costs in Healthcare?
Key cost-saving mechanisms:
- Automating routine administrative tasks
- Improving diagnostic accuracy and reducing unnecessary tests
- Enabling preventive interventions before conditions become costly to treat
- Optimising resource allocation across healthcare systems
The economics: In financial terms, AI’s impact on healthcare costs is substantial. The Department of Health and Social Care estimates that AI applications could save the NHS approximately £12.5 billion annually by 2030—about 10% of its current operating budget.
These savings come through multiple channels. Administrative AI streamlines operations by automating appointment scheduling, billing, and documentation, potentially reducing administrative costs by up to 30%. Diagnostic AI helps prevent costly medical errors and unnecessary procedures, while predictive analytics identifies high-risk patients for preventive intervention before they require expensive emergency care.
Perhaps most significantly, AI enables more personalised treatment approaches. By analysing individual patient characteristics, algorithms can help identify which treatments are most likely to succeed for specific patients, reducing costly trial-and-error approaches and minimising adverse reactions. This precision medicine approach not only improves outcomes but also eliminates spending on treatments unlikely to benefit particular patients.
Conclusion
“The future of healthcare isn’t artificial intelligence alone, but intelligent collaboration between human expertise and technology.”
The story of AI in healthcare isn’t one of miraculous solutions or dystopian replacement—it’s about augmentation, efficiency, and expanding what’s possible in medicine. The most successful implementations recognise both AI’s remarkable capabilities and its limitations, pairing technological innovation with human expertise.
As patients and healthcare consumers, understanding the realistic potential of AI helps us engage more productively with these emerging technologies. We can advocate for responsible innovation that prioritises both clinical outcomes and ethical considerations.
The future of healthcare won’t be built entirely on algorithms, nor will it ignore their transformative potential. Instead, it will thoughtfully integrate AI capabilities into systems that remain fundamentally human-centred. In this balanced approach lies the true promise of artificial intelligence in healthcare—not as a replacement for medical professionals, but as a powerful ally in their vital work.





