Healthcare organisations across the globe continue to face a silent but costly challenge: healthcare revenue leakage. Hospitals and clinics deliver quality care every day, yet inaccurate claims, delayed reimbursements, and manual billing gaps quietly drain financial resources. These losses limit growth, restrict technology investments, and reduce funds available for patient care.
Modern healthcare leaders now turn to AI medical billing and AI-driven claims management to protect revenue, improve accuracy, and strengthen financial performance. This blog explains how hospital revenue cycle AI helps global hospitals and clinics eliminate revenue leaks, improve ROI, and create sustainable financial resilience—without requiring deep technical expertise.
Executive Summary: Why Healthcare Revenue Leakage Demands Immediate Action
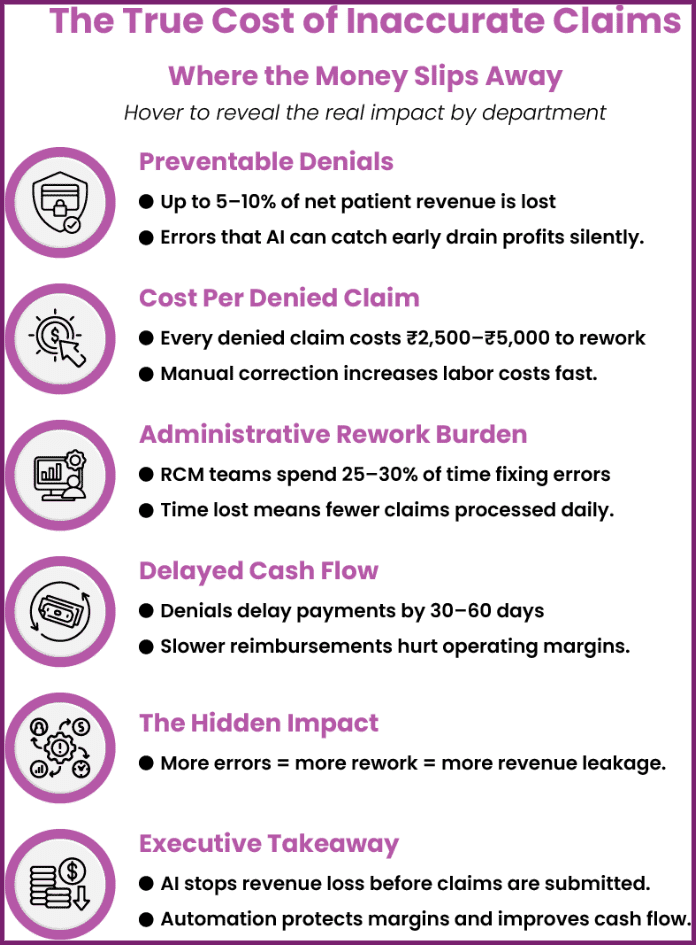
Healthcare organisations operate on thin margins. Even small inefficiencies in claims processing result in significant financial losses at scale. Healthcare revenue leakage often occurs invisibly through coding inaccuracies, missed charges, claim denials, and delayed payments.
Traditional medical billing solutions struggle to manage today’s complex payer rules and growing claim volumes. Hospitals that rely on manual workflows experience rising denials and unpredictable cash flow. Automated medical billing powered by AI transforms this challenge into an opportunity. AI identifies errors early, improves claims accuracy, and strengthens revenue integrity across the entire billing lifecycle.
Understanding Healthcare Revenue Leakage in Simple Terms
What Is Healthcare Revenue Leakage?
Healthcare revenue leakage refers to earned revenue that hospitals never collect. Organisations lose this revenue through billing errors, under-coded services, incomplete documentation, and rejected claims. These losses do not appear as obvious failures, which makes them harder to detect and fix.
Common Causes of Revenue Leakage Across Global Hospitals
Hospitals worldwide experience revenue leakage due to:
- Manual billing and coding mistakes
- Incomplete clinical documentation
- Inconsistent payer-specific rules
- Fragmented systems across departments
- Reactive denial management processes
Without hospital revenue cycle automation, these issues multiply as claim volumes grow.
Also Read – What is Revenue Leakage in Healthcare & How To Reduce It? – Ezovion.
The Real Impact of Healthcare Revenue Leakage on Hospitals and Clinics
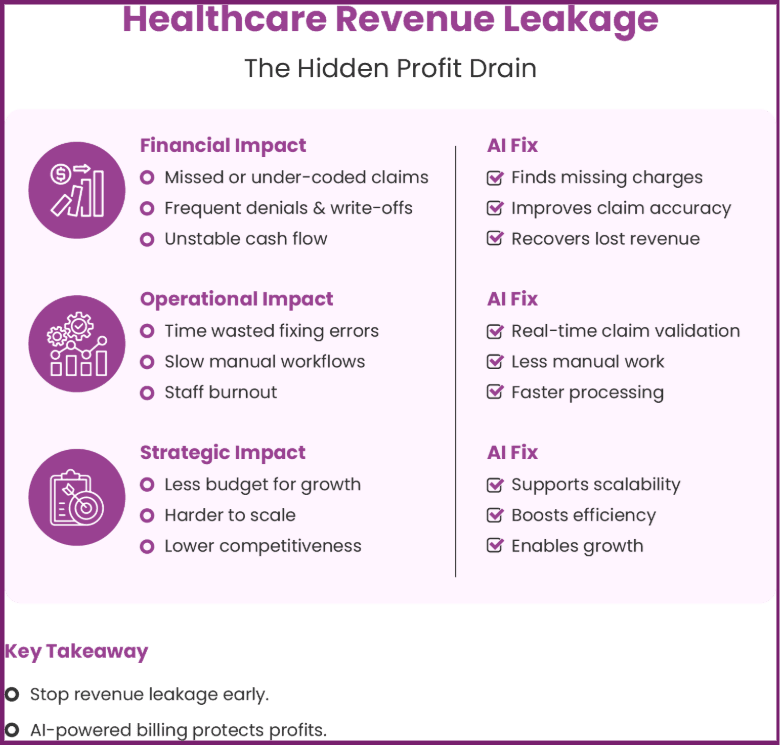
• Financial Consequences
Healthcare revenue leakage directly reduces reimbursements by allowing billable services to go unclaimed, under-coded, or denied. Over time, these losses accumulate into significant write-offs that weaken financial stability. Hospitals also experience unpredictable cash flow, which makes budgeting and long-term planning difficult. Manual billing workflows often fail to identify errors before claim submission, leading to delayed payments and costly rework.
Hospital revenue cycle AI, supported by AI medical billing and AI-driven claims management, proactively identifies missing charges and coding inconsistencies. By improving claims accuracy at the source, automated medical billing and modern medical billing solutions help hospitals recover revenue that traditional processes consistently overlook.
• Operational Consequences
Revenue leakage increases operational strain on billing and revenue cycle teams. Staff spend excessive time correcting denied or rejected claims instead of preventing errors early. This reactive approach leads to burnout, lower productivity, and longer claim turnaround times. As claim volumes grow, manual processes become unsustainable.
Healthcare RCM automation streamlines workflows by validating claims in real time and reducing dependency on repetitive manual checks. AI medical billing enables billing teams to work efficiently while maintaining high accuracy and consistency across payers.
• Strategic Consequences
Persistent revenue leakage limits a hospital’s ability to invest in innovation, infrastructure upgrades, and workforce development. Organisations that rely on outdated billing systems struggle to scale operations and adapt to changing reimbursement models. Without automated medical billing and intelligent medical billing solutions, hospitals lose competitiveness in an increasingly data-driven healthcare environment.
Why Traditional Medical Billing Solutions Fall Short
Manual and Rule-Based Billing Systems
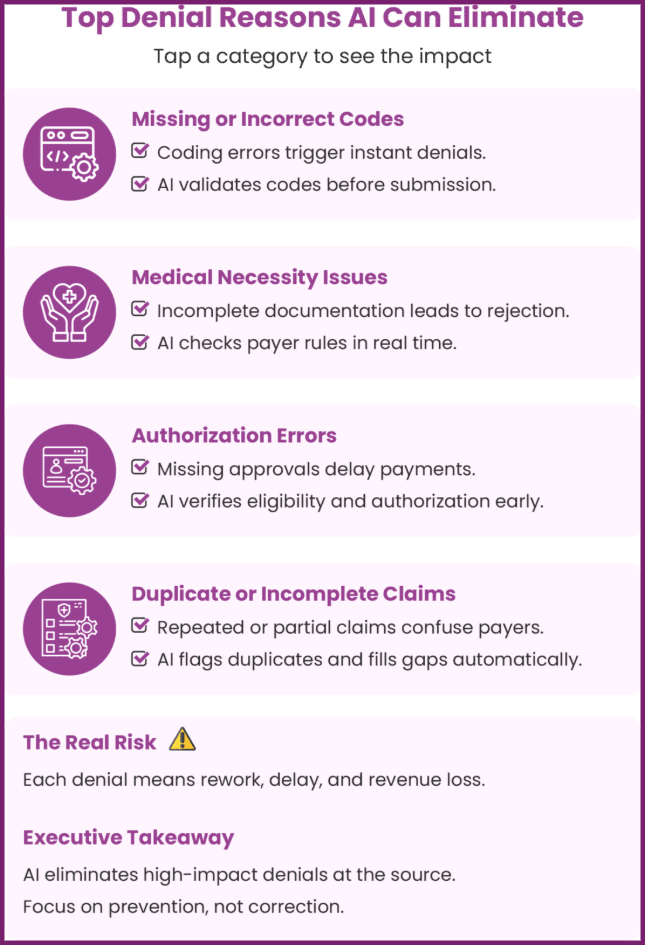
Legacy billing platforms depend heavily on static rules and manual intervention. These systems react to denials after submission instead of preventing them. As payer rules change, manual systems fall behind.
Growing Complexity in Healthcare Claims
Payers continuously update reimbursement policies. Hospitals manage multiple contracts, regions, and regulations. AI in healthcare claims processing provides continuous learning and adapts to this complexity in real time.
Also Read – Steps To Prevent Revenue Leakage In Healthcare
AI Medical Billing Explained Without Technical Jargon
AI medical billing simplifies complex healthcare billing processes by using intelligent technology to prevent errors before they impact revenue. Instead of relying on manual checks, AI medical billing continuously reviews billing data, clinical documentation, and payer-specific rules in real time.
This approach helps hospitals reduce healthcare revenue leakage, improve medical claims accuracy, and strengthen overall hospital revenue cycle AI performance. By embedding intelligence directly into everyday workflows, automated medical billing enables healthcare organisations to achieve higher reimbursement rates without increasing administrative burden.
What AI Medical Billing Really Means
AI medical billing uses advanced algorithms to examine large volumes of billing and clinical data and identify patterns that commonly cause claim rejections or underpayments. These systems automatically verify codes, documentation completeness, and payer compliance before claims reach insurers. As a result, AI-driven claims management helps hospitals prevent costly errors, support AI in healthcare claims processing, and ensure consistent, accurate submissions across the entire medical billing solutions lifecycle.
How AI Supports Billing Teams
AI enhances human expertise rather than replacing it. Through AI-driven claims management, billing teams receive real-time guidance, automated validations, and early risk alerts that improve confidence and efficiency. Hospital revenue cycle automation allows teams to focus on strategic tasks while AI handles repetitive checks. This collaboration helps organisations reduce claim denials in healthcare, streamline workflows, and protect revenue without requiring staff to master complex technology.
How AI-Driven Claims Management Actively Blocks Revenue Leaks
Revenue leakage in healthcare quietly erodes profitability by letting hospitals and clinics lose money at multiple points in the revenue cycle — from inaccurate billing and unsubmitted charges to rejected insurance claims and under-payments. These hidden losses make it harder to sustain operations, reduce funds available for growth, and shrink operating margins over time — often without administrators even realising it until financial reports reveal a shortfall.
Integrating an intelligent Hospital Information Management System (HIMS) like Ezovion directly tackles these issues by tightening every part of the revenue cycle, improving claim success rates, accelerating reimbursements, and ultimately boosting profitability through better financial control and insight.
• Preventing Errors Before Claim Submission
Automated medical billing within Ezovion HIMS validates codes, documentation, and payer requirements before claims leave the system. This AI-powered verification ensures completeness and consistency, significantly improving medical claims accuracy and reducing rework.
By catching potential errors before submission, hospitals avoid the costly cycle of corrections and resubmissions — minimising claim denials, reducing administrative spend, and protecting revenue that otherwise would have leaked due to simple documentation mistakes.
• Reducing Claim Denials at the Source
Hospitals that use AI in healthcare claims processing achieve higher first-pass acceptance rates. Ezovion’s intelligent system identifies denial risks early — including mismatched codes, missing documentation, or payer compliance issues — and equips teams to correct them proactively.
This early mitigation reduces claim denials in healthcare consistently, shortens payment turnaround times, and strengthens overall cash flow. As denials shrink, so do the hidden costs associated with review cycles and write-offs, enabling clinics and hospitals to retain more of the revenue generated from services already delivered.
• Identifying Hidden Revenue Opportunities
AI analyses historical claims and identifies under-coded services, missed charges, and overlooked billable procedures. Ezovion HIMS’s advanced billing insights make it possible for hospitals to capture full reimbursement for the care they provide.
By uncovering revenue opportunities that traditional manual systems miss, healthcare practices unlock additional profit streams — turning previously lost or invisible revenue into recognised income. Over time, this deep billing intelligence enhances decision-making, strengthens financial planning, and improves operational transparency across departments.
Profit Impact & What Hospital and Clinic Owners Experience with Ezovion HIMS
By choosing Ezovion HIMS:
• Revenue leakage is dramatically reduced — when billing, coding, and claim validation are automated and aligned with payer requirements.
• Profitability improves through faster reimbursement cycles, fewer denials, and reduced administrative costs.
• Operational efficiency increases — staff spend less time on manual corrections and more time on strategic tasks that drive growth.
• Real-time financial insights and dashboards give owners immediate visibility into accounts receivable, departmental performance, and revenue trends — enabling proactive financial decisions instead of reactive firefighting.
• Full revenue capture is achieved by identifying previously unbilled services and correcting under-coding issues automatically, translating directly into higher net revenue.
In sum, revenue leakage doesn’t just reduce profitability — it erodes the financial foundation of healthcare practices. Ezovion HIMS actively plugs these leaks, turning inefficiencies into profit drivers and transforming billing and claims management into a source of financial strength for hospitals and clinics.
Also Read – Revenue Cycle Management Healthcare – Ezovion.
The ROI of Hospital Revenue Cycle AI
Financial Gains from Automated Accuracy
Hospitals that deploy hospital revenue cycle AI experience faster reimbursements and reduced leakage. Medical billing solutions powered by AI improve cash flow predictability and financial stability.
Operational Efficiency at Scale
Hospital revenue cycle automation reduces manual workloads and improves staff efficiency. Teams focus on value-added activities instead of repetitive corrections.
Long-Term Revenue Protection
AI creates a preventive revenue strategy. Hospitals avoid future losses by addressing issues before they impact reimbursements.
Global Use Cases: How Hospitals and Clinics Benefit
Large Multi-Speciality Hospitals
High-volume hospitals rely on AI-driven claims management to maintain consistency across departments. AI ensures standardised billing practices and supports enterprise-scale accuracy.
Mid-Sized Hospitals and Clinics
Smaller organisations maximise revenue with limited staff through automated medical billing. AI delivers enterprise-level intelligence without large operational costs.
Multi-Location Healthcare Networks
Networks benefit from centralised healthcare RCM automation that ensures consistent claims accuracy across regions and payer environments.
Addressing Common Concerns About AI Adoption
• “Our Team Is Not Technology-Friendly”
AI platforms offer intuitive dashboards and simple workflows. Hospitals deploy AI medical billing without extensive training or disruption.
• “Will AI Replace Our Existing Systems?”
Modern medical billing solutions integrate seamlessly with existing HIS and RCM platforms. Hospitals enhance current systems instead of replacing them.
• “Can We Trust AI with Compliance?”
AI supports compliance through continuous monitoring and audit-ready documentation. AI in healthcare claims processing improves accuracy while meeting regulatory requirements.
Building a Future-Proof Revenue Strategy with Hospital Revenue Cycle AI
Shifting from Reactive to Preventive Revenue Management
Hospitals move from fixing denied claims to preventing errors entirely. Hospital revenue cycle AI creates proactive revenue protection.
Scaling Financial Performance with Confidence
AI adapts as organisations grow. Hospitals expand services and regions without increasing billing complexity or risk.
Also Read – The Importance of HIMS Software In Healthcare Analytics – Ezovion.
Turning Claims Accuracy into a Strategic Advantage
Hospitals and clinics can no longer afford revenue leakage in an increasingly complex healthcare environment. AI medical billing, medical billing solutions, and hospital revenue cycle AI provide a clear path to accuracy, efficiency, and financial resilience.
By adopting AI in healthcare claims processing, organisations strengthen medical claims accuracy, consistently reduce claim denials in healthcare, and secure long-term financial health. AI transforms claim accuracy from an operational task into a strategic advantage that fuels growth, innovation, and better patient care.





