In the bustling corridors of hospitals and the quiet sanctuaries of patient homes, a silent force works tirelessly, shaping the very trajectory of healing. They are the caregivers – the unsung heroes who bridge the gap between medical intervention and holistic recovery. More than just helping hands, they are the pillars of support, the watchful eyes, and the comforting presence that transforms patient care.
For hospitals and patient care clinics, understanding and valuing the caregiver role is not just good practice; it’s essential for achieving optimal patient outcomes and fostering successful patient recovery. This blog delves into the indispensable contributions of caregivers, exploring how their involvement profoundly impacts patient journeys, both within hospital walls and beyond.
The Indispensable Partnership: Caregivers as Integral Care Team Members
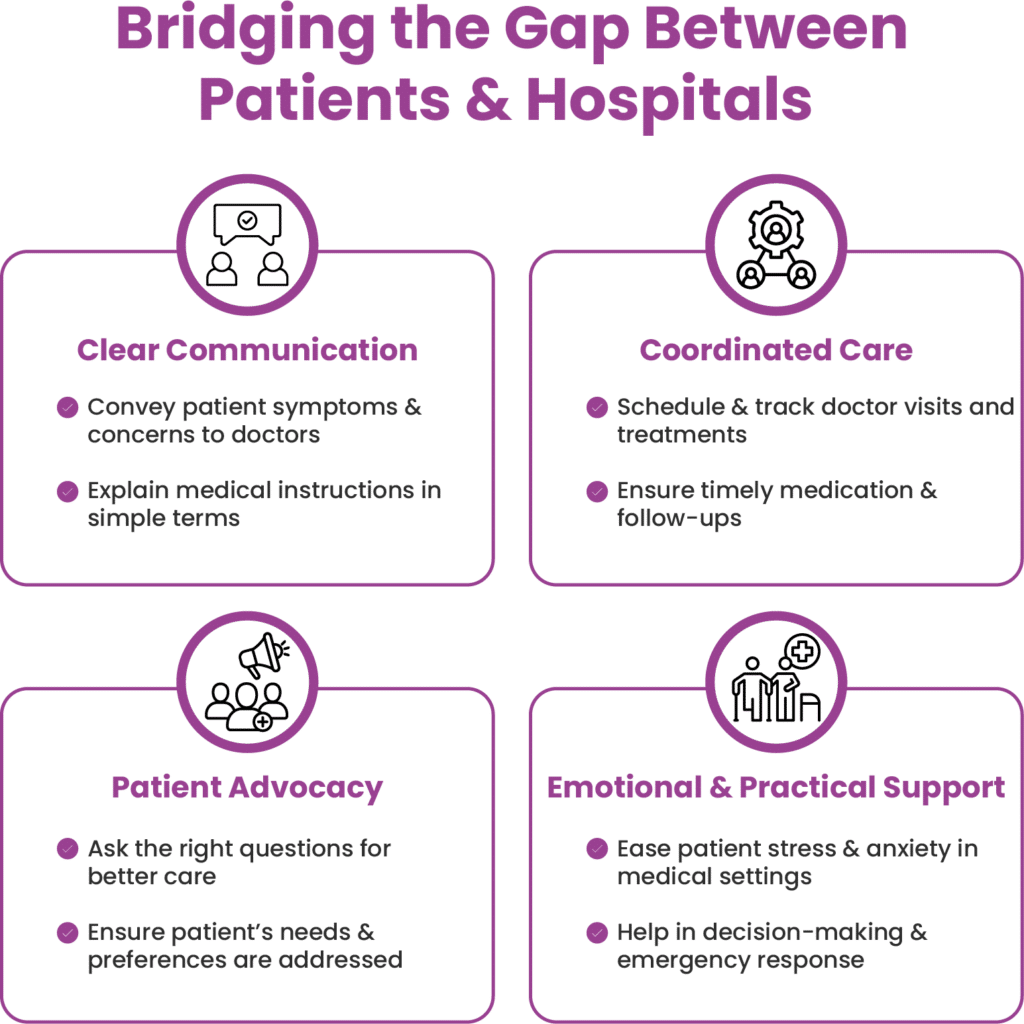
Hospitals and clinics must recognise that caregivers are not merely visitors; they are integral members of the care team. Their intimate knowledge of the patient, their ability to provide emotional support, and their dedication to ensuring adherence to treatment plans are invaluable assets. Patient-centred care thrives when caregivers are actively involved, creating a holistic approach that addresses not just physical needs but also emotional and social well-being.
1. Active Participation in Treatment Plans
Caregivers act as an extension of medical professionals by ensuring that treatment plans prescribed by doctors are followed accurately. They provide supportive and communicate clearly by:
• Keeping track of medications and dosages.
• Monitoring patient symptoms and side effects.
• Ensuring coordinated care through regular follow-ups and doctor visits.
• Helping patients adhere to dietary and lifestyle changes through patient advocacy.
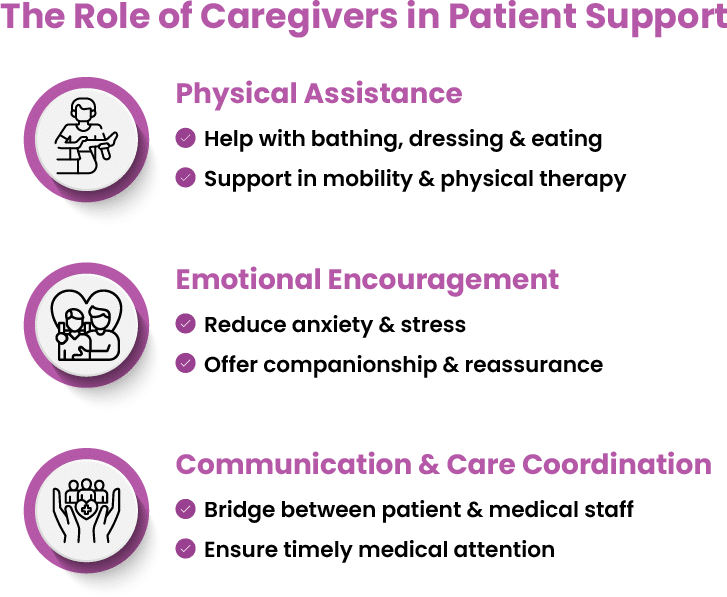
2. Providing Physical and Emotional Support
Patients recovering from illnesses often require both physical assistance and emotional encouragement as well as support. Caregivers help in giving the necessary emotional and practical support by:
• Assisting in daily activities like bathing, dressing, and eating.
• Encouraging physical therapy and mobility exercises.
• Providing emotional support to reduce anxiety and stress.
• Acting as a point of contact between the patient and medical staff.
3. Preparing for Hospital Discharge and Home Care
One of the most critical moments in a patient’s journey is transitioning from the hospital to home. The impact of family caregivers on hospital discharge cannot be underestimated. Hospitals and clinics must educate caregivers on:
• Post-discharge care instructions and medications.
• Recognising warning signs of complications.
• Scheduling follow-up appointments.
• Creating a safe home environment for recovery.
Decoding the Caregiver’s Impact: A Step-by-Step Guide
1. Active Participation in Decision Making
Caregivers are often the patient’s strongest advocates. Their presence during consultations ensures that vital information is understood and remembered.
By actively participating in decision-making, they help patients make informed choices about their treatment, leading to better adherence and improved outcomes. This is a core part of supportive care. Hospitals must encourage open communication, ensuring caregivers are included in discussions about treatment plans, medications, and follow-up care.
2. Ensuring Medication Adherence
Caregivers play a crucial role in monitoring medication schedules, ensuring patients take their prescribed dosages correctly and on time. This is especially vital for patients with chronic conditions or complex medication regimens. Clinics should provide clear instructions and resources to caregivers, empowering them to manage medications effectively.
3. Providing Physical Support
From assisting with mobility and personal hygiene to helping with daily tasks, caregivers provide essential physical support. This is particularly important for patients recovering from surgery or managing disabilities. Hospitals can offer training and guidance to caregivers on safe lifting techniques and other practical skills.
4. Offering Emotional Support
The emotional toll of illness or injury can be immense. Caregivers provide a vital source of comfort, encouragement, and companionship, reducing anxiety and promoting a positive outlook. Supportive care includes recognising and addressing the emotional needs of both patients and caregivers.
5. Monitoring Symptoms and Changes
Caregivers are often the first to notice subtle changes in a patient’s condition. Their keen observation and timely reporting can prevent complications and ensure prompt medical intervention. Hospitals should educate caregivers on recognising warning signs and reporting changes to healthcare professionals.
6. Facilitating Communication
Caregivers act as intermediaries between patients and healthcare providers, ensuring clear and effective communication. They can articulate the patient’s concerns and relay important information. This communication is essential for patient-centred care, and to get the best patient recovery.
7. Promoting a Safe Home Environment
After hospital discharge, caregivers play a crucial role in creating a safe and supportive home environment. This includes ensuring proper hygiene, managing medical equipment, and preventing falls. The impact of family caregivers on hospital discharge is immense, as the home environment is a crucial step in the patient’s recovery.
A 2022 meta-analysis of 54 studies involving over 31,000 individuals demonstrated that active caregiver involvement during transitions between healthcare settings (e.g., from hospital to home) is instrumental in preventing rehospitalizations and improving patient outcomes.
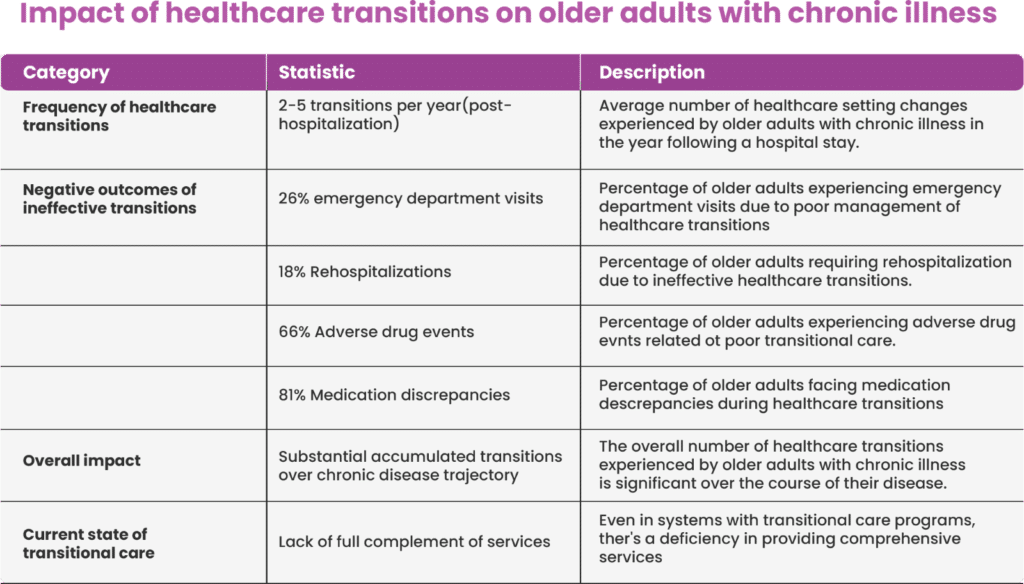
As per the above table, a significant percentage (26%) of emergency department visits among older adults with chronic illnesses are attributed to poor management of these healthcare transitions. This suggests that inadequate communication, lack of follow-up care, or insufficient preparation for the next care setting can lead to complications requiring emergency medical attention.
Similarly, 18% of rehospitalizations for this population are due to ineffective healthcare transitions. This highlights that when transitions are not handled well, patients are more likely to experience issues that necessitate a return to the hospital. A concerningly high percentage (66%) of adverse drug events (negative reactions to medications) experienced by older adults are related to poor transitional care. This often stems from medication errors, lack of reconciliation of medication lists across different settings, or inadequate patient education about their medications.
Large majority (81%) of older adults face discrepancies in their medication lists during healthcare transitions. This means there are inconsistencies in the medications they are supposed to be taking, including differences in dosages, frequencies, or even the medications themselves, as they move between different healthcare settings. Substantial accumulated transitions over chronic disease trajectory can be burdensome, confusing, and increase the risk of negative outcomes if not properly managed.
The Hospital Discharge and Beyond
The transition from hospital to home is a critical phase. The caregiver role is vital in ensuring a smooth and safe discharge. Hospitals should:
• Provide comprehensive discharge planning, including clear instructions for caregivers.
• Offer training and resources to help caregivers manage post-discharge care.
• Establish ongoing communication channels for caregivers to seek support and guidance.
• The caregiver support in this transition phase heavily influences the patient recovery.
• How caregivers improve patient outcomes during the transition is a key point to understand.
Empowering Caregivers: A Shared Responsibility
Recognising the caregiver role as an essential component of patient care is not just a compassionate gesture; it’s a strategic imperative. Hospitals and clinics must invest in caregiver support, providing education, resources, and respite care. By empowering caregivers, healthcare providers can enhance patient outcomes, improve efficiency, and foster a more holistic approach to healing.
The Heart of Healing: Celebrating the Caregiver’s Contribution
In the complex tapestry of healthcare, caregivers are the threads that weave together compassion, dedication, and unwavering support. Their contribution is immeasurable, their impact profound. By acknowledging and valuing their role, hospitals and clinics can unlock the true potential of patient-centred care, transforming healing journeys and enriching lives. Their efforts truly make a difference in patient recovery and in the achievement of positive patient outcomes.





