
Healthcare enterprises face intense pressure to deliver consistent performance, manage fluctuating demand, and stabilise financial outcomes. Leaders across major health systems now treat hospital capacity management as a core strategic function rather than an operational afterthought. Executives want predictable workflows, strong profitability, and coordinated system-wide operations. This shift creates a powerful need for reliable capacity planning in hospitals, efficient resource allocation, and enterprise-driven decision-making.
The New Strategic Imperative for Hospital Capacity Management
Healthcare enterprises now treat hospital related capacity management as a mission-critical priority because they want consistent performance, predictable workflows, and enterprise-wide operational stability. With rising patient volumes, staffing constraints, and growing financial pressures, leaders rely on strong capacity planning in hospitals to anticipate demand and manage resources with precision. They view capacity as a strategic asset that directly influences quality, revenue, and system-wide resilience.
As organisations expand across regions and service lines, executives integrate hospital capacity management into long-term planning, digital transformation initiatives, and daily operational decision-making. This shift elevates capacity management from a tactical function to a central driver of competitiveness, sustainability, and high-value healthcare delivery.
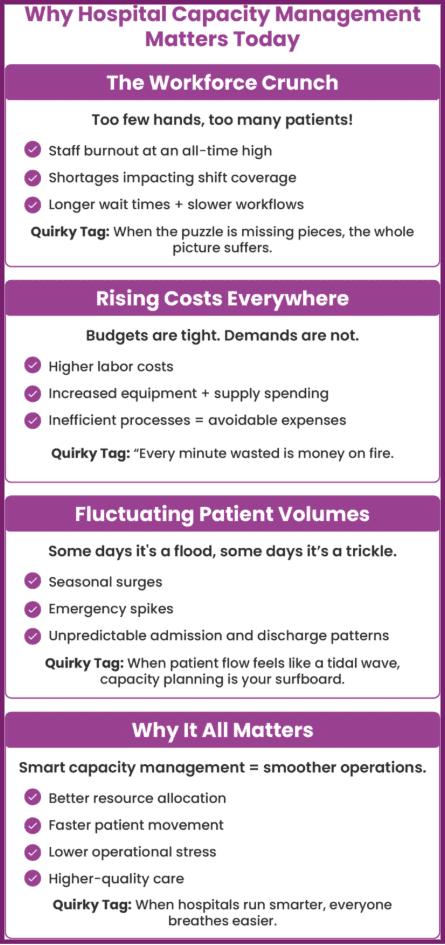
Why Healthcare Enterprises Prioritise Hospital Capacity Management
Healthcare leaders want to strengthen system efficiency without compromising care quality. They treat hospital capacity activities as a strategic engine that supports every high-value goal, from financial performance to patient outcomes. They also apply strong capacity planning in hospitals to forecast demand and guide operational adjustments in real time. Executives rely on hospital capacity optimisation to align staffing, beds, and clinical resources with projected patient needs. They build unified strategies because this approach strengthens hospital operations efficiency across every campus in their network.
Business Impact of Capacity Planning in Hospitals
Enterprise hospitals face unpredictable surges, changing case complexity, and seasonal variation. Leaders use capacity planning in hospitals to bring order to this uncertainty. Their models incorporate length of stay prediction, demand forecasting, and operational triggers that guide proactive actions. They empower administrators through decision-support systems for hospital administrators that visualise capacity metrics, patient flow patterns, and throughput barriers. These enterprise-level capabilities demonstrate how hospital capacity management improves financial performance by reducing overtime labour, optimising resource distribution, and lowering variation across facilities.
Key Enterprise Value Drivers of Strategic Hospital Capacity Management
Healthcare enterprises treat hospital-related capacity management as a core growth engine because it directly enhances hospital operations’ al related capacity management as a core growth engine because it directly enhances hospital operations efficiency, improves financial stability, and strengthens system-wide performance. Leaders rely on strong capacity planning in hospitals and data-driven models to manage demand, optimise resources, and maintain operational predictability across diverse care settings. With advanced hospital capacity optimisation and a unified hospital capacity planning strategy, health systems unlock measurable value through better patient flow, smarter workforce alignment, and more balanced network utilisation.
Revenue Growth Through Strategic Patient Placement
Enterprise hospitals strengthen revenue by using strategic hospital capacity solutions for health systems to balance patient placement across their network. Leaders analyse transfer needs, speciality availability, and acuity levels to move patients to the most suitable site. They increase throughput in high-value departments by applying advanced hospital capacity optimisation models. Their teams use hospital capacity planning strategy frameworks to reduce delays that affect bed availability. They improve enterprise visibility through decision-support systems for hospital administrators, allowing them to choose optimal patient destinations and eliminate bottlenecks.
Also Read – Why Hospital Software Integration Is The Backbone Of Hospital Growth – Ezovion
Operating Cost Reduction and Workforce Stability
Strong hospital capacity management frameworks reduce excessive labour spending. Leaders deploy real-time dashboards that merge resource data, length of stay prediction insights, and staffing needs. These tools showcase how hospital capacity work improves financial performance by reducing contract labour use and eliminating inefficient scheduling practices. Health systems use hospital operations efficiency programs to ensure right-sized staffing at every hour of the day. They also prepare for seasonal spikes by activating structured hospital surge capacity management plans that prevent financial leakage.
Quality Improvement and Better Patient Flow
High-performing enterprises use capacity planning in hospitals to elevate care experiences. Their flow teams monitor demand variations, acuity changes, and patient movement across departments. They integrate hospital capacity planning strategy models that shorten wait times, improve discharge predictability, and streamline care transitions. Their predictive tools combine length of stay prediction and clinical decision rules, giving them confidence to adjust workflows in real time. These improvements strengthen hospital operations efficiency across emergency care, acute units, and surgical departments.
Organizational Factors That Influence Hospital Capacity Management Success
Scale, Structure, and System Integration
Large health systems need cohesive strategies to align facilities that differ in size and speciality. Executives unify processes through standardised hospital capacity planning strategy models that guide daily workflow decisions. They use decision-support systems for hospital administrators to centralise operational visibility. These systems track capacity-related KPIs and show how hospital capacity solutions improves financial performance through optimised placement decisions.
Also Read – Revolutionizing Healthcare: The Power of Hospital Information System – Ezovion
Geographical and Resource Variability
Health systems operate in urban, suburban, and rural markets. Leaders use enterprise-wide capacity planning in hospitals to manage these geographic differences. They deploy hospital surge capacity management tools that help smaller facilities handle sudden volume spikes. They adopt strategic hospital capacity management for health systems, so every location contributes to unified outcomes.
Governance and Cultural Alignment
Executives create empowered command centres that run hospital capacity operations. They encourage collaboration between nursing, emergency teams, speciality departments, and transfer centres. They reinforce these efforts through sophisticated decision-support systems for hospital administrators, which boost transparency and system alignment.
Also Read – Centralized Hospital Management System By Ezovion.
Implementation Roadmap for Strategic Hospital Capacity Management
A structured implementation roadmap helps healthcare enterprises strengthen hospital management by aligning capacity planning in hospitals, advanced analytics, and operational workflows with a scalable hospital capacity planning strategy that drives hospital operations efficiency, enhances hospital capacity optimisation, and supports system-wide decision making through modern decision-support systems for hospital administrators.
Phase 1: Assessment and Planning
Leaders begin with a complete assessment of bed demand, staffing patterns, service line performance, and historical flow metrics. They incorporate length of stay prediction models and throughput analyses to support strong hospital capacity planning strategy development. They review data to identify where hospital capacity optimisation can produce rapid wins.
Phase 2: Operating Model and Technology Enablement
Executives create centralised capacity teams that monitor enterprise performance and coordinate actions across multiple campuses. They use digital platforms that improve hospital operations efficiency by combining forecasting models, capacity planning in hospitals, and real-time bed visibility. These platforms integrate decision-support systems for hospital administrators that guide safe placement decisions and enhance standardisation. Leaders also build enterprise frameworks that demonstrate how hospital capacity management improves financial performance.
Phase 3: Enterprise Execution and Scaling
Hospitals run pilot programs in high-pressure areas such as EDs and surgical floors. They refine processes based on findings and scale them across the enterprise. Their models incorporate hospital surge capacity management rules that ensure resiliency during peak demand. They strengthen operational predictability by integrating hospital capacity optimisation practices that address bottlenecks and reduce variation across facilities.
Also Read – The Impact of AI on Hospital Management: What You Should Know
Measuring the ROI of Hospital Capacity Management
Tracking Enterprise KPIs
Executives evaluate outcomes using standardised KPIs that measure throughput, occupancy, and efficiency. They monitor length of stay prediction accuracy, discharge timing, and staffing alignment. These metrics show how hospital management improves financial performance by revealing reductions in overtime labour, decreased diversion rates, and maximised revenue from high-value service lines.
Financial and Operational Impact Across Health Systems
Health systems report measurable gains after adopting strategic hospital capacity management for health systems frameworks. They reduce unnecessary admissions, increase patient flow speed, and improve physician availability. Their commitment to continuous improvement strengthens enterprise-wide growth.
Also Read – The Impact Of Value-Based Care on Hospital Operations and How We Help Succeed – Ezovion.
The Future of Hospital Capacity Management in Enterprise Healthcare
Healthcare enterprises now rely on advanced hospital capacity management and capacity planning in hospitals to drive hospital capacity optimisation, strengthen hospital operations efficiency, and support long-term resilience through predictive analytics and data-driven decision-support systems for hospital administrators.
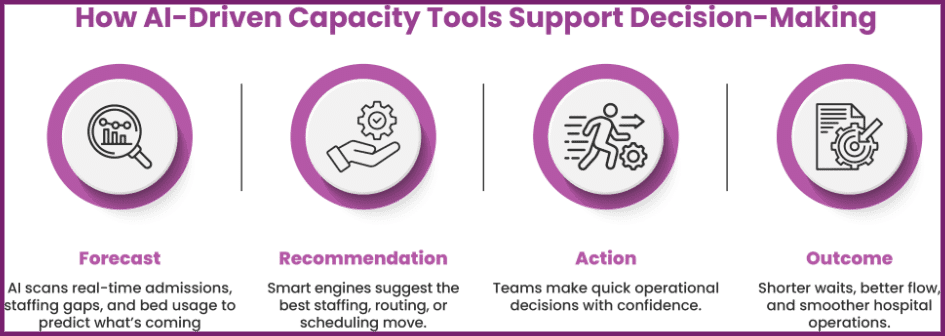
Predictive Models, AI, and Automation
AI-driven forecasting enhances hospital capacity optimisation by predicting demand spikes, resource shortages, and bottlenecks. Health systems apply these tools to refine capacity planning in hospitals and strengthen long-term strategies. Executives gain deeper insights through decision-support systems for hospital administrators, which help them make faster and more accurate operational decisions.
Surge Planning and Enterprise Resilience
Predictive modelling strengthens hospital surge capacity management and enables rapid adjustments during crises. Large systems unify their response strategies and prevent operational breakdowns.
The Strategic Future of Capacity Planning in Hospitals
Healthcare enterprises treat hospital capacity management as a top strategic priority because they want predictable performance, greater profitability, and smooth operations across every facility. Strong capacity planning in hospitals helps leaders anticipate demand, guide efficient workflows, and support sustainable growth.
Enterprise-driven models demonstrate how hospital capacity management improves financial performance, stabilises workforce planning, and enhances care quality. Organisations that adopt a robust hospital capacity planning strategy position themselves for long-term success, regardless of future challenges.





